An aortic aneurysm is the enlargement of the aorta either in the chest or abdomen before it branches into other parts of the body. Aortic aneurysms are a vascular issue that can affect people with other health or lifestyle behaviors that lead to high blood pressure or cardiovascular stress. Aortic aneurysms are also more common with increasing age. Other risk factors for aneurysms include a history of tobacco use, high blood pressure, connective tissue disorders, or family members with aneurysms. If the aneurysm is large or growing rapidly, treatment options include the use of fabric covered stents or open surgery to prevent or treat aortic rupture. Brian Rubin, MD is an expert in the repair of aortic aneurysms using open surgery and endovascular (stenting) techniques.
On this page:
Aortic Aneurysms and Surgery: Frequently Asked Questions
What is an aortic aneurysm?
An aortic aneurysm is a balloon-like enlargement of the aorta. The aorta is a large vessel that branches off the heart and supplies the body with oxygenated blood. Aortic aneurysms are difficult to detect without screening, but they are deadly if allowed to progress and even rupture, leading to internal bleeding.
What kinds of aortic aneurysms exist?
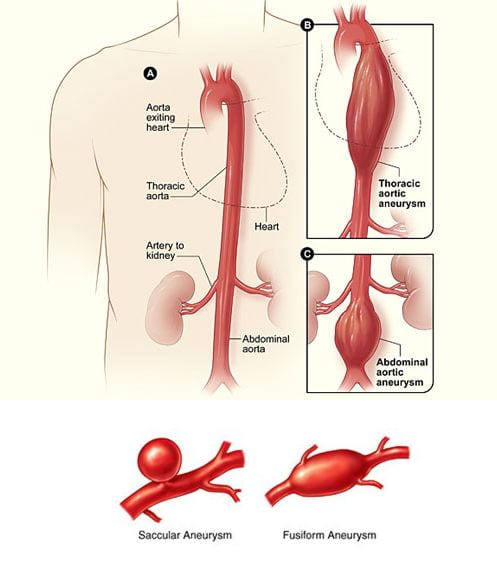
Two main forms of aortic aneurysm are recognized based on their placement along the length of the aorta vessel. A thoracic aortic aneurysm (TAA) occurs in the chest, in the ascending or descending thoracic region of the aorta. The other type is an abdominal aortic aneurysm (AAA). These aneurysms are characterized by bulging in the aorta as it progresses into the abdomen, below the diaphragm (the muscle sheet separating the chest and abdominal cavities). AAAs are more common than TAAs. Aneurysms can also span from the chest into the abdomen, called thoracoabdominal aneurysms.
Aortic aneurysms can also be classified by their shape. Fusiform-shaped aneurysms bulge or balloon out from the aorta in a relatively symmetrical way. They are the more common form. Saccular-shaped aneurysms bulge or distend from only to one side of the aorta, making the vessel asymmetrical.
How is an aortic dissection different from an aneurysm? How dangerous are these conditions?
“Aortic dissection is another aortic disease with many of the same potential risks as an aneurysm,” Dr. Rubin adds. “Dissection most often occurs in patients with underlying abnormalities of the tissues of the aortic wall or high blood pressure.”
Complications from a dissection include the enlargement of the aorta into an aneurysm. Aortic dissection can also lead to partial tears in the wall of the aorta, limiting blood flow beyond the dissection as the aorta branches into the body. This complication diverts proper blood circulation and reduces the dispersal of oxygen and nutrients to organs and body systems.
Aortic aneurysms and dissections are dangerous and potentially deadly if allowed to progress. The risk of rupture is largely correlated with aneurysm size or the severity of dissection. If an aneurysm or dissection bursts, causing bleeding into the body cavity around the aorta, this is called a rupture. A ruptured aortic aneurysm can cause massive, often fatal internal bleeding.
What are the symptoms of an aortic aneurysm? What does an aortic aneurysm feel like?
Most aneurysms cause no symptoms and are discovered on radiology studies conducted for other health and wellness reasons. When symptoms do occur, the location of the aneurysm can determine how they present. Thoracic aortic aneurysms have symptoms like sharp, sudden chest or upper back pain. Abdominal aortic aneurysms are less likely to have detectable symptoms before they pose a serious threat, such as rapid expansion or rupture. A patient may experience throbbing or pain in the back or side of their abdomen, along with pain in the legs, groin, or buttocks. Some symptoms may resemble other conditions like coronary artery disease, gastric reflux or peptic ulcer disease.
In the case of a dissection or rupture, the patient might feel like they are having a heart attack or stroke. Sudden, severe chest pain is the number one symptom for aortic rupture. A drop in blood pressure and symptoms of shock will follow. Aortic aneurysms can also affect people with no symptoms until they rupture, presenting a higher mortality risk.
What causes aortic aneurysms?
The risk factors for aortic aneurysms include smoking, high blood pressure (hypertension), high cholesterol, and inflammatory conditions. Inherited genetic factors can also increase the likelihood of developing aortic aneurysms.
Thoracic aortic aneurysms are most often caused by cystic medial degeneration, which is the breakdown of the aortic vessel wall. TAAs can also occur due to high blood pressure or acute injury to the aorta. TAAs are more common among people with increasing age, family history of TAAs or genetic disorders affecting connective tissue. They are distributed equally among sexes. Abdominal aortic aneurysms more often develop in males and those older than 65. AAAs are also statistically more common than TAAs.
Aneurysm ruptures can result from long-term or acute stress on the aneurysm. Long-term cardiovascular issues or the continued stress of unhealthy lifestyle behaviors contribute to damage in the aortic muscle walls, eventually causing failure. Acute triggers can also incite a rupture; a weakened aortic aneurysm can rupture from extremely demanding physical activity or medication that causes an increase in blood pressure or heart activity.
Are aortic aneurysms hereditary?
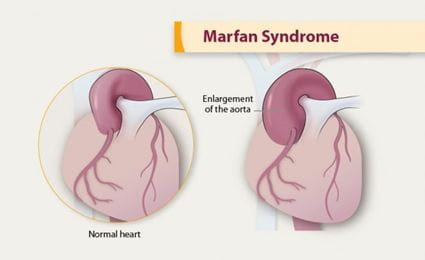
There are several inherited health disorders that may contribute to the development of aortic aneurysms. Connective tissue disorders, including Marfan syndrome and Ehlers-Danlos syndrome, can increase a patient’s risk of aortic aneurysms. In Marfan syndrome, there is a higher tendency for the development of thoracic aortic aneurysms and aortic dissection; for those with Ehlers-Danlos syndrome, the likelihood for aortic rupture is higher. A general family history of aortic aneurysms can also indicate elevated risk.
How common are aortic aneurysms?
The frequency of aortic aneurysm increases with age and other confounding health problems relating to the cardiovascular system. Abdominal aortic aneurysms occur in around 1–9% in males and around 1–2% in females per screening statistics. Thoracic aortic aneurysms are less common than AAAs, with an occurrence rate of 5-10 out of 100,000 persons per year.
How is an aortic aneurysm detected?
An aortic aneurysm may be detected during a routine medical screen or imaging test, such as an x-ray, CT scan or ultrasound on the chest or heart. Specific screening for aortic aneurysms involves patient history and a physical examination as well as testing to visualize potential ballooning of the aorta. Diagnostic imaging tests may include radiological scans like ultrasound, CT or CAT, MRI, and angiogram.
How are aortic aneurysms treated? What size aortic aneurysm requires surgery?
“The decision to treat an aneurysm is based on both its size (diameter), shape and location,” explains Dr. Rubin. “Many aneurysms are small and require only follow-up ultrasound or CT scans to monitor their size. If aneurysms are large or show evidence of rapid enlargement or rupture, treatment is necessary to remove or reinforce the damaged region of the aorta.”
Aortic aneurysms are mediated through medicines and surgery. Medicines can lower blood pressure and reduce the risk of an aortic aneurysm occurring. Medication can also lessen an established aneurysm’s ability to progress, dissect or rupture.
In more severe aneurysms, surgery can repair or replace the affected section of the aorta. Advanced aneurysms – those that are larger than 4-5.5 centimeters or have damaged the aortic wall – are more likely to require surgery, as they pose a more direct threat to the health of the patient. If the aneurysm is causing pain or growing quickly, preventative surgery is also the best treatment route. Acute dissection or rupture of the aneurysm is an emergency and requires immediate surgery.
Treatment type will be determined based on the patient’s condition and the presentation of the aneurysm. Age, overall health, medical history and tolerance of certain treatments will be considered. Further thought is given to the extent of the aneurysm, the symptoms it is causing and expectations for how it may progress.

What kind of surgery repairs an aortic aneurysm? How long does it take?
The aneurysm’s severity and location will determine the route of surgery and how long it takes. Open surgical repair or endovascular repair are available. Open surgical repair, either in the chest or abdomen, removes the part of the aorta with the aneurysm, which is then replaced with a graft. Open surgical repair is the more traditional form of surgery and will be necessary for severe aneurysms and ruptures. The process can take two to six hours to complete.
“Endovascular repair is an option for thoracic and abdominal aortic aneurysms and aortic dissections.” Dr. Rubin, who specializes in both procedures, explains that endovascular repair is conducted through smaller incisions within an access vessel, usually the common femoral artery, through which a stent graft component is inserted and moved up to the aneurysm site. A stent graft is composed of a metal mesh tube (stent) and thin fabric (graft). The stent graft is placed in the affected area to reinforce the aortic wall, preventing further stress from causing more damage. Endovascular repair methods are less invasive and have a lower risk of complications and takes somewhere between two and four hours.
How long is recovery from surgery?
o The extent of the surgery will impact the length of time it takes for a patient to fully heal. Open surgical repair will require a 4-6 day hospital stay, followed by a recovery period of 6 weeks to 3 months before the patient fully returns to normal activities. Endovascular repair requires only one or two days in the hospital, and full recovery can be shortened to as little as a week but may be longer for some patients.
Washington University Aortic Aneurysm Surgeons
The team of Washington University vascular surgeons, including Dr. Rubin, are highly trained in the most advanced techniques for repairing aortic aneurysms. They see patients at the Center for Advanced Medicine Heart & Vascular Center, Barnes-Jewish West County Hospital and Christian Hospital. Endovascular and open repair surgeons provide expert surgical care for patients with aortic aneurysms.
You can follow the Vascular Surgery team on Twitter for news in the field and treatment of aortic aneurysms and other cardiovascular illness.
For more information about aortic aneurysm surgery or to make an appointment with Dr. Rubin at the Center for Advanced Medicine Heart and Vascular Center or Barnes-Jewish West County Hospital, please call 314-747-8272.
For more information or to make an appointment at Christian Hospital, visit the Christian Hospital website or call 314-747-9355.