On Wednesday, August 31, faculty and trainees of the Washington University Department of Surgery and Division of Cardiothoracic Surgery gathered for the long-awaited second annual Nicholas T. Kouchoukos Research Day, presented by the Foundation for Barnes-Jewish Hospital. Five Washington University cardiothoracic trainees – Postdoctoral Research Associate Khashayar Farahnak, MD; Research Fellow Martha McGilvray, MD, MSt; Research Fellow Hailey Shepherd, MD; Postdoctoral Research Scholar Tari-Ann Yates, MD; and Postdoctoral Research Associate Yuhei Yokohama, MD – delivered presentations to an audience of Washington University faculty, staff and trainees – including Kouchoukos himself. Visiting professor Ankit Bharat, MD, of Northwestern University concluded the event with a lecture describing the importance and concrete results of persistent and creative research efforts in the cardiothoracic medical field.
The Nicholas T. Kouchoukos Research Day was established to honor Dr. Kouchoukos’ legacy as a dedicated researcher and clinician and to exhibit the commitment and innovations of current Washington University cardiothoracic trainees. His philanthropy carries on his legacy and continues to support the academic mission of Washington University through the Kouchoukos Research Fellowship.

Farahnak kicked off the event with his a presentation entitled “Role of B Cells in Primary Graft Dysfunction after Lung Transplantation.” Farahnak worked closely with his mentor, Ruben Nava, MD, over the past year in his research and discovered a correlation between the presence of B cells and higher amounts of classical monocytes recruitment and neutrophil extravasation in human lungs post-transplant. These findings lay the groundwork for potential future therapeutic treatments which would target and deplete B cells, potentially reducing the risk of extravasation in lung transplant patients.
McGilvray delivered the second presentation, entitled “Understanding How Chronic Severe Mitral Regurgitation Leads to Mechanical and Electrical Remodeling of the Canine Heart.” She described her extensive two-year study, conducted under the mentorship of Chief of Cardiothoracic Surgery and Evarts A. Graham Professor of Surgery Ralph Damiano, Jr., MD, which worked toward developing a model of the effects of severe mitral regurgitation in canines for future application in human medicine. These efforts proved successful: Kouchoukos personally congratulated McGilvray on creating such an accurate model.
Shepherd, a research fellow of G. Alexander Patterson, MD/Mid-America Transplant Endowed Distinguished Chair in Lung Transplantation Daniel Kreisel, MD, PhD, presented her research on “Mechanisms Contributing to the Development of Pleural Fibrosis Following Pulmonary Transplantation.” This study investigated possible contributing factors to pleural fibrosis in the lungs. Her findings illustrated that hyaluronic acid accumulates in grafts very quickly after transplant and that this accumulation may lead to notable fibrotic remodeling and irreversible injury to the lung. This study opens the door for further experimentation and research exploring this pathway and potential treatments inhibiting hyaluronic acid to help prevent fibrosis and injury after lung transplant.
Yates’ presentation, entitled “Long Term Rhythm and Survival Outcomes in Patients with Atrial Fibrillation and Mitral Valve Disease Who Underwent the Concomitant Cox Maze IV Procedure,” examined some of the outcomes of the Cox-maze IV procedure – an innovation pioneered at Washington University by Yates’ mentor, Damiano. Yates’ study examined perioperative outcomes and complications in patients undergoing this procedure concomitantly with other cardiac surgeries and found that these patients demonstrate better long-term survival and no increase in 30-day mortality and pacemaker placement as opposed to patients who forewent the Cox-maze IV.
Read more: Atrial Fibrillation at a Glance
The final presentation of the day, entitled “Mechanisms of Extravasation of CD8 T Cells After Lung Transplantation,” was delivered by Yokohama, a postdoctoral research associate of Dr. Kreisel. This study sought to examine and define mechanisms that promote CD8 T infiltration into lung allografts and explored pathways which inhibit extravasation.
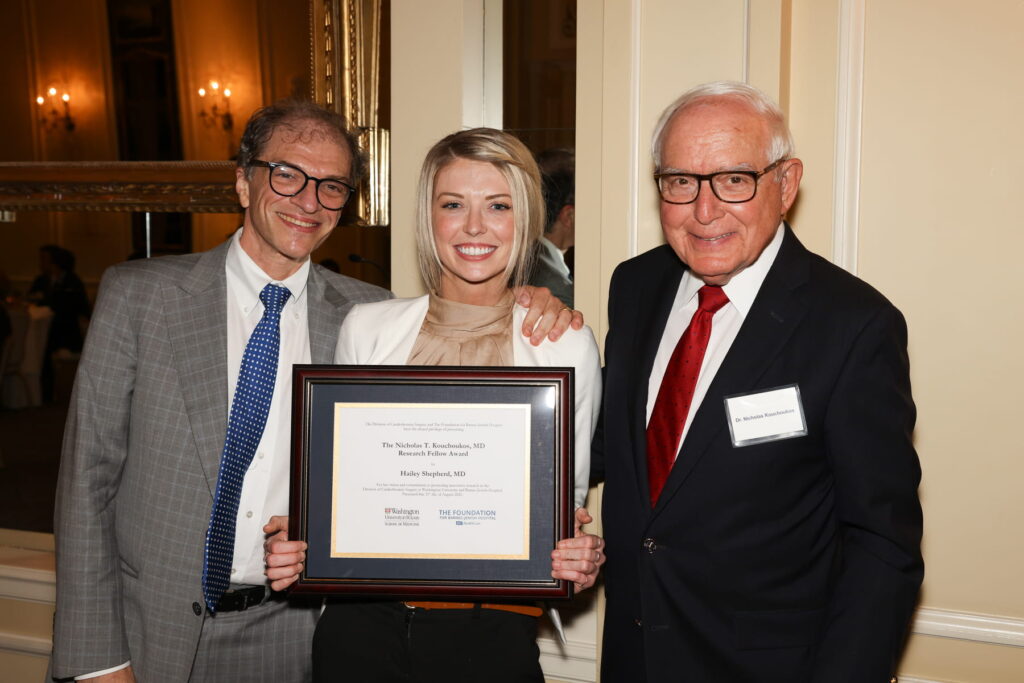
After an afternoon of exemplary presentations and lectures, a jury of four judges, including Kouchoukos, were tasked with determining the recipient of the second annual Nicholas T. Kouchoukos, MD, Research Fellow Award. The recipient was determined based off based off the participant’s concept, delivery and ability to discuss their research and findings. Out of the five trainees, the jury awarded Shepherd for her excellent research and presentation. Shepherd’s passion, creativity and persistence in her research embody the legacy of Dr. Kouchoukos and his bold and groundbreaking contributions to the specialty. Following her presentation, Joseph Bancroft Professor of Surgery G. Alexander Patterson, MD, applauded Shepherd’s tenacity. “You’re not the first person who had a novel idea met with skepticism,” he told Shepherd. “Terrific presentation.”
Following the five trainee presentations, visiting professor Ankit Bharat, MD, a physician well associated with advocating for his own novel ideas when met with skepticism, delivered a lecture entitled “Problem Based Surgical Research.” Bharat, an alum of the general surgery and cardiothoracic surgery residencies and postdoctoral fellowship at Washington University School of Medicine, is the Harold L. and Margaret N. Method Professor of Surgery, Chief of Thoracic Surgery and Executive Director of the newly-founded Canning Thoracic Institute at Northwestern University. His lecture incorporated three stories from his clinical practice involving infection, technology and COVID-19. He discussed what he learned participating in the first lung transplant at Northwestern University, his experiences in experimenting with technology to improve monitoring and treatment and how he and his team handled, learned from and adapted to the COIVD-19 crisis in Chicago.
Throughout his lecture, Bharat highlighted the importance of building trust across the entire medical team. He noted that this trust is vital when it comes to implementing a new clinical idea and that innovations in medicine come with time and persistence. “I remind myself that a good clinician or surgeon is not one that can make decisions in the presence of evidence,” Bharat concluded, “it is one who can make good decisions in the absence of evidence.”
For over 40 years, Dr. Kouchoukos, now professor emeritus in the Division of Cardiothoracic Surgery, has been a pioneer at the forefront of cardiothoracic medicine at Washington University and beyond. He earned his medical degree at Washington University, where he worked in laboratories with renowned surgeons Thomas B. Ferguson, MD, and Charles L. Roper, MD, who fostered his growth as a student and encouraged him to pursue cardiothoracic surgery as a specialty. His accomplishments have contributed significantly to the advancement of cardiothoracic medicine, most notably including his development of the modified Bentall procedure. Kouchoukos boldly pioneered revolutionary ideas and advocated research which lead to ground-breaking advances in patient care and cardiothoracic medicine. “We owe a lot to the early pioneers like Dr. Kouchoukos,” said Damiano.