For people with chronic pancreatitis, pain is almost constant and treatment options are limited. Surgeons in the Hepatobiliary-Pancreatic and Gastrointestinal (HPB-GI) Surgery Section at Washington University School of Medicine in St. Louis specialize in disorders of the liver, pancreas and GI tract, including pancreatitis. HPB surgeon Chet Hammill, MD, MCR, has introduced a procedure that can help cure some people of chronic pancreatitis.
The pancreas is the gland that makes insulin and enzymes that aid in digestion. Pancreatitis is inflammation of the pancreas, which occurs when the enzymes in the pancreas cause damage to the pancreas itself.
According to the National Institute of Diabetes and Digestive and Kidney Diseases, pancreatitis is becoming increasingly common, with about 275,000 hospital stays for acute pancreatitis in the United States every year.
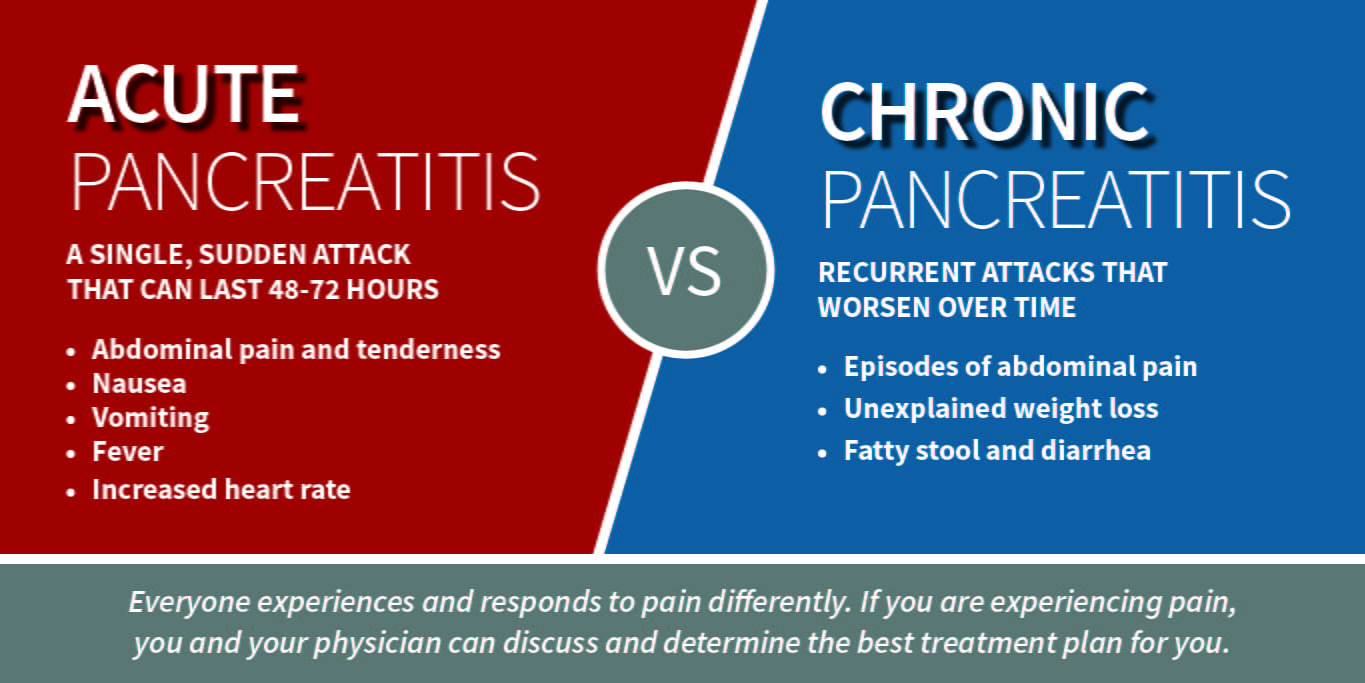
Acute pancreatitis is a single attack, whereas chronic pancreatitis involves recurrent attacks that get worse with time and can cause permanent damage to the pancreas.
“For acute pancreatitis, we manage the symptoms and provide nutritional support to help the patient heal,” Hammill says. “When we see someone with pancreatitis, we figure out the cause or trigger for their attack and eliminate the risk factors. A second episode of acute pancreatitis is more likely to cause a chronic problem for that person.”
The most common cause of pancreatitis is gallstones, which occur when substances in the gallbladder harden, blocking the flow of fluids that aid in digestion. Men are more likely than women to get pancreatitis, and other risk factors include abdominal fat, high triglycerides and diabetes. Alcohol use is listed as a common risk factor, though Hammill notes that data suggest smoking is more likely to put someone at risk of pancreatitis.
A New Cure
One treatment for chronic pancreatitis is removal of the pancreas, called total pancreatectomy. By removing the source of the pain, pancreatectomy can effectively “cure” the person of pancreatitis. The trouble with removing the whole pancreas is that, without their pancreas, the person has no way of producing insulin.
“If you don’t have insulin, you have diabetes,” Hammill explains. “Total pancreatectomy trades off pain for a very difficult to manage type of diabetes.”
The alternative to surgery is pain management with narcotics, which can cause addiction and do not address the cause of the pancreatitis.
For some people with chronic pancreatitis, there is another option that can treat the pain and reduce the risk of developing brittle diabetes.
Total pancreatectomy and islet auto-transplant (TP-IAT) takes the cells responsible for producing insulin, called islet cells, from the removed pancreas, and puts them in the person’s liver. By returning the islet cells to the body, TP-IAT allows the person to continue producing insulin naturally.
“The hope is that they don’t get diabetes,” Hammill says.
The outcome depends on how much functional pancreas the person has at the time of surgery. Pancreatitis damages the pancreas, so the sooner the disease is caught, the better the chance of harvesting islet cells. If the yield of islet cells is high enough, TP-IAT can cure a person of the pain of pancreatitis without leading to diabetes.
“For young patients with a genetic predisposition causing their pancreatitis, who would have a long, painful course, this is really a good option to control the pain and maintain their quality of life,” Hammill says.
From Mars to Medicine
HPB surgeons at the School of Medicine see patients for the full spectrum of liver, pancreas, gallbladder and GI disorders. The HPB-GI Section has acquired a national reputation as one of the highest-volume liver and pancreas surgery sections in the United States. Hammill sees many patients with liver, pancreas or bile duct cancer. Among non-cancerous conditions, pancreatitis is one of the most common he treats.
Hammill brings expertise in minimally invasive techniques to complex HPB surgeries. He completed fellowship training in Hepatobiliary and Pancreas Surgery at Portland Providence Medical Center. As a general surgery resident at University of Hawaii, Hammill developed a clinical interest in minimally invasive surgery. He has combined these areas of expertise to bring a growing number of minimally invasive techniques to the traditionally large and complex cases seen in HPB surgery.
“HPB is classically known for big surgeries, like the Whipple surgery,” Hammill acknowledges. “But we are able to offer minimally invasive Whipple surgery, distal pancreatectomy, liver resections and other HPB surgeries at the School of Medicine.”
Hammill has always known he wanted to help people, but his path to surgery is, in his own words, “a little complex.”
Before he was a surgeon, Hammill worked as an aerospace engineer. He earned a Master of Science in Aeronautical and Astronautical Engineering from the University of Illinois, then worked for years on advanced life support for space travel.
“I was working on research, finding ways to keep people alive on trips to Mars,” Hammill recalls. While the results of the work were rewarding, he was not satisfied spending his days in front of a computer. “It’s not where I imagined myself. I wanted to have more of a direct impact on peoples’ lives.”
For Hammill, that direct impact was through medicine. He earned his medical degree despite not having the premed background many of his fellow students possessed. In medical school, he had to work harder than most, but that hard work led him to a rewarding career in the challenging field of HPB surgery.
“I took an unusual path, but I’ve figured out where I’m supposed to be,” Hammill says.
The Sooner the Better
TP-IAT is a new procedure to the School of Medicine—one offered at only a select few centers across the country—although islet transplant has a long history at Washington University.
“The concept of harvesting islets was developed here at Washington University by the pathologist Paul Lacy,” Hammill says.
From bench to bedside, this research led to islet transplants from pancreas donors. The next step, auto-transplant, was more complex because of the challenges involved in collecting a high yield of islets from a single person’s pancreas. Islet auto-transplant is not an option at most centers because of the challenges involved in running a lab capable of harvesting the cells.
Through industry partnership, the Department of Surgery is now able to offer TP-IAT for eligible people with chronic pancreatitis early in the disease process. Hammill emphasizes the importance of catching this problem while there are still enough islet cells in the pancreas.
“There is an option,” Hammill says. “If you are young, with new chronic pancreatitis, don’t wait until later to start looking for options. The earlier we can take care of this problem, the better the outcome can be in the long run.”
