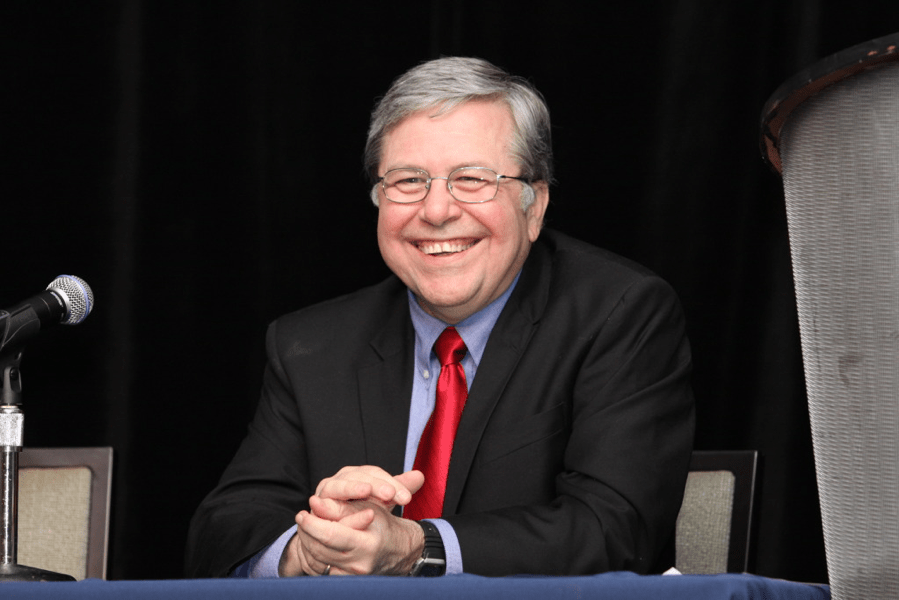
Richard Schuessler, PhD, Director of the Cardiac Surgical Research Laboratory, retires from the Department of Surgery in October 2020, after an accomplished 35-year career at Washington University School of Medicine in St. Louis.
Professor of Surgery & Biomedical Engineering at the School of Medicine, Schuessler’s focus was on the surgical treatment of cardiac arrhythmias.
Schuessler worked with James Cox, MD, former Division Chief of Cardiothoracic Surgery, the late John Boineau, MD, Professor of Surgery, Medicine and Biomedical Engineering, and Ralph J. Damiano, Jr., MD, Evarts A. Graham Professor and Chief of Cardiothoracic Surgery, to address problems with cardiac arrhythmia and electrophysiology. Schuessler’s contributions were instrumental in the development of the Cox-Maze procedure—the first cure for atrial fibrillation.
As laboratory director, Schuessler also served as a teacher and mentor for the many students, residents and research fellows who have worked in the Cardiothoracic Surgery Research Laboratory over the years.
“It’s been a wonderful career,” Schuessler reflects. “I’ve worked with a lot of great people.”
Cutting His Teeth in Bioengineering
Schuessler grew up in St. Louis, the son of a mechanical engineer, and studied mathematics at University of Missouri—Rolla in the 1970s, earning a BS and MS in Computer Science. His interest was not in “computers for computers’ sake,” but in numerical analysis and differential equations.
The math Schuessler took became so complex and abstract that it was difficult to explain it to peers outside of his classes. As he completed graduate school at Rolla in 1974, Schuessler craved something more applied. He was still interested in solving complex math problems, but wanted to use that knowledge for a more practical application.
At around that time, Schuessler saw a brochure for a PhD program in bioengineering at Clemson University in South Carolina. Much of the foundation for bioengineering and electrophysiology was rooted in mathematics similar to what Schuessler had studied at Rolla, but this program would allow him to work on research that could help improve lives.
Schuessler applied and was accepted He planned to begin that fall semester. But then came a twist:
“Someone from the faculty called me one day and said, ‘We have a summer assistantship available. Would you want to start early?’ I said that sounded fine. ‘When do you want me to start?’ This was a Friday,” Schuessler recalls.
The Clemson faculty member asked: “Can you be here Monday?”
“I got into my car and drove,” Schuessler says. “I called my girlfriend, who is now my wife of 45 years, and told her where I was going. Her family got out their road map and could not find Clemson, South Carolina, so there was a lot of suspicion!”
Recounting this story now, over 45 years later, Schuessler laughs. He describes the challenges of moving hundreds of miles across the country for a PhD program in a single weekend, all with the smile and good humor that his colleagues have come to recognize him for.
Schuessler’s first project was not in the heart, but in teeth. He was working on finite stress analysis of a new kind of dental implant—essentially trying to create a stronger post for more stable artificial teeth. Parts of this project required Schuessler to travel roughly 100 miles from Clemson to the Medical College of Georgia. It was at the Medical College of Georgia, during his PhD studies at Clemson University, that Schuessler met John Boineau, who would become his long-time mentor in cardiac research.
“Dr. Boineau was a pioneer in basic and clinical electrophysiology,” Schuessler says. “He recognized that only by recording potentials directly for the heart could the basis of the electrocardiogram and mechanisms of arrhythmias be understood.”
Boineau was at the forefront of the surgical treatment of Wolf-Parkinson-White syndrome, a condition affecting the electrical conduction system of the heart. Because of Schuessler’s interest in electrophysiology, joining Boineau’s laboratory after graduation was a natural fit. Schuessler received a National Research Service Award (NRSA) from the National Institutes of Health (NIH), funding his research with Boineau.
The Archimedes Moment
“I made a decision early in life that I was only going to work with people smarter than me,” Schuessler says, “and Washington University is a great place for that.”
Schuessler’s relationship with the university goes back more than 60 years. His father graduated from Washington University in 1950, earning a BS in Mechanical Engineering. Schuessler recalls visiting the campus as a young boy, attending engineering days and witnessing the thriving academic community he would eventually join.
Schuessler, together with Boineau, came to Washington University in 1984. The two were recruited by the new Division Chief of Cardiothoracic Surgery, James Cox. It turned out that Boineau had been Cox’s mentor in electrophysiology at Duke University in the 1960s, more than ten years before providing similar mentorship to Schuessler in Georgia. Now that Cox was at the School of Medicine, he wanted to bring the best researchers in cardiac surgery to his division. Thanks to these decades-spanning connections, Boineau, Cox and Schuessler made contributions to several of the most serious and complex cardiac conditions.
“When I was at Duke,” Cox recalls, “we had developed surgical procedures to treat basically all cardiac arrhythmias except atrial fibrillation.” Now at Washington University, with an all-star team of researchers, the Cardiac Surgical Research Laboratory focused on finding a surgical cure for atrial fibrillation (AF).
AF is a type of cardiac arrhythmia in which, according to the Centers for Disease Control and Prevention (CDC), “the normal beating in the upper chambers of the heart (the two atria) is irregular, and blood doesn’t flow as well as it should from the atria to the lower chambers of the heart (the two ventricles).” The CDC estimates that between 2.7 and 6.1 million people in the United States have AF. Symptoms of AF include irregular heartbeat, heart palpitations, lightheadedness, extreme fatigue, shortness of breath and chest pain, and the American Heart Association notes that AF increases a person’s risk of stroke.
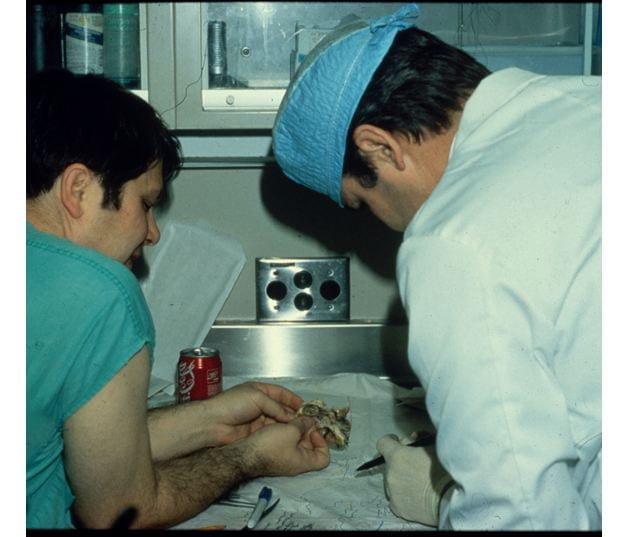
Schuessler and Boineau used new developments in mapping and imaging technology to better understand what AF looked like in the heart, and what it would take to make the heart beat normally again. Their experiments produced results that looked chaotic and confusing at first glance. It took diligence and attention to detail, as well as several iterations of their research model to understand what was really happening in the heart when AF was present. Finally, Schuessler and Boineau made sense of the complex data, seeing how AF occurred and what specific areas of the heart were affected.
When the research team showed Cox their findings, he said: “I can fix that.”
The treatment, known as the Cox-Maze Procedure, involves making a series of safe and effective scars to permanently block the electrical signals triggering the irregular heartbeat.
“Not many times in your career do you actually get an Archimedes ‘Eureka’ moment,” Schuessler says. The breakthrough moments in Schuessler’s long and accomplished research career have led to a greater understanding of the heart’s electrophysiology and the surgical treatment of problems with cardiac arrhythmias. “It’s been very gratifying to see something so successful for the treatment of atrial fibrillation.”
A New Phase of Innovation
In 2000, Schuessler began a new phase of collaboration when Damiano joined Washington University as the John M. Shoenberg Professor and Chief of Cardiac Surgery. Damiano’s interest in the surgical treatment of arrhythmias began during medical school and surgical training at Duke, where he was Cox’s research fellow and the recipient of an NRSA for his work on the surgical treatment of arrhythmias. Damiano’s arrival in the Department of Surgery brought together Cox’s mentor, Boineau, and two of his mentees—Schuessler and Damiano—under one roof.
“It was a dream come true to come to St. Louis and work with Boineau and Schuessler, two of the giants in the field of arrhythmia surgery,” Damiano recalls. “Their pioneering work led to the development of this entire area of cardiac surgery, and their laboratory was the pre-eminent surgical electrophysiology research unit in the world.”
Over the next 20 years, this team continued to innovate and modify the pioneering work the of the Cox-Maze procedure.
“We saw an opportunity to make what was a very complex and difficult operation more accessible to all practicing cardiac surgeons,” Schuessler says.
This development led to the Cox-Maze IV procedure, a less invasive, more widely used procedure that is now the gold standard for the surgical treatment of atrial fibrillation, and the only operation to receive an FDA indication for the treatment of atrial fibrillation.
“With the help of Dr. Schuessler’s insight and scientific prowess, we rigorously evaluated new ablation devices and developed a foundation for progress,” Damiano asserts. “After extensive investigation, we developed an ablation lesion set that closely mirrored the cut and sew Cox Maze III procedure. We have shown that this procedure has had similar success rates with significantly lower morbidity and mortality. Dr. Schuessler oversaw and directed not only the experimental work, but also the evaluation of our clinical innovations. This made a rarely performed operation accessible to most surgeons in the world. The annual number of cases grew from several hundred in the 1990s to almost 50,000 last year.”
Damiano especially appreciates Schuessler’s role in mentoring and training residents as future surgeon/scientists. Schuessler has provided oversight for the division’s T32 Basic Science Research Training grant, which has funded over 100 fellow positions, including nine who are former or current faculty at Washington University.
“Rick was not only a great scientist, but equally excelled as a teacher of medical students, research fellows and faculty,” Damiano says. “Over the years, he trained residents from the United States and all over the world that would go back to leadership positions at their own institutions. They have unanimously expressed to me their loyalty to Dr. Schuessler and gratitude for all that he taught them.”
Over a long and successful career in research, Schuessler’s contributions have deeply impacted all who have worked with him.
“There is no doubt in my mind that Dr. Schuessler is a pre-eminent scientist and teacher who was instrumental to the development of the field of surgical treatment of arrhythmias. However, perhaps more importantly than his scientific contributions, his real legacy is the wonderful research and training environment that he developed at Washington University,” Damiano reflects. “We are all proud, not only to have worked with him as a colleague, but to have greatly benefited from his friendship and mentorship over the years. His unique combination of intelligence, insight, compassion and integrity will be sorely missed and extremely difficult to replace.”

Not a Sprint, But a Marathon
One of the proudest moments of Schuessler’s career was finding that the surgical treatment of AF led to patients living longer. A medical student in the laboratory measured outcomes, comparing patients who had received the Cox-Maze Procedure to those who had not, and found the survival rate of patients whose AF had been treated was significantly higher.
“We knew we were getting rid of the AF, but this showed us that people were living longer,” Schuessler asserts. “That’s been one of the more rewarding things of my career: that we actually helped people, and people lived longer because of what we did.”
This, like the many other discoveries of the research laboratory, was made possible by the students under Schuessler’s mentorship. The researchers, whether undergraduates, medical students, residents or research fellows, are the true workhorses of the laboratory, according to Schuessler.
“On a day-to-day basis,” he says, “these researchers are doing the hard work of creating research models, collecting tissue from the operating room, recording data from patients or following up with patients. My job over the years has been to facilitate that work. I tease a lot of them by saying that my greatest contribution to their research is to stay out of their way—and that’s hard to do sometimes.”
The laboratory has 2 objectives:
- To solve the clinical problems that face cardiac and thoracic surgery.
- To train the future researchers who will carry on and be the academicians of the future.
“I hope my legacy is all of the people we have trained over the years,” Schuessler says. “I’ll miss the people most of all. Working with medical students and undergraduates has kept me in a delayed adolescence,” he says with a laugh. “In some ways, I’m still back in college with these young men and women, and somehow I don’t feel like ‘the old guy’ when I’m with them.”
Schuessler’s curiosity, jovial personality and intellect will be greatly missed as well.
Though he will miss the laboratory and researchers, Schuessler is eager to see the great accomplishments that the laboratory will go on to produce under new leadership.
Christian Zemlin, PhD, joins the faculty as new Director of the Cardiac Surgical Research Laboratory, continuing NIH-funded AF and enabling the Division of Cardiothoracic Surgery to establish a strong relationship with the Biomedical Engineering School of Washington University by offering biomedical engineering students a defined program in the laboratory. Zemlin earned his PhD in Theoretical Physics from Humboldt University in Berlin and postdoctoral research in Cardiac Electrophysiology at SUNY Upstate Medical University in Syracuse, New York before joining Washington University.
“I expect bigger and better things in the future,” Schuessler affirms. “This is a great environment with strong leadership. Ralph Damiano has done an amazing job. The clinical case-load has increased here while in many places it has gone down. Our surgeons are doing cutting-edge work, addressing the difficult clinical problems that need to be solved.”
Schuessler recognizes that he is fortunate to have seen the fruits of his labor in AF reach clinical application. The difficult thing about research is that the clinical applications can take a lot of time to manifest, and many researchers do not see that end result in the course of their career.
“Jim Cox always used to comment that research isn’t a sprint, it’s a marathon,” Schuessler remembers. “And sometimes the marathon is pretty long—a lot more than 26 miles. “
Schuessler knows this well: research he published on artificial teeth while at Clemson seemed to go unnoticed for decades. In recent years, however, he has been cited over 140 times for this publication. Sometimes, Schuessler says with a laugh, he still gets calls asking him to submit to dental research journals, which he politely declines.
“When you are in medical research, one thing you have to recognize is that a lot of what you do may have impact, but it might be 50 years before it has impact, or it may be peripheral to patient outcomes. I know people who have spent their entire career doing wonderful research, but haven’t seen the impact,” Schuessler acknowledges. “I always tell fellows: It might take a while, but maybe that research will have impact.”
Work hard, be patient and follow the scientific method, Schuessler advises, and your efforts will help you reach the finish line in the long marathon of a research career.
Now that he has crossed that finish line, Schuessler looks forward to spending time with his wife—who was an administrator for the laboratory until her retirement this Feb.—traveling, visiting national parks, practicing photography, and staying busy with his grandchildren.