Lung transplants can improve the quality of life for people with severe or advanced chronic lung conditions, such as chronic obstructive pulmonary disease (COPD), cystic fibrosis and pulmonary fibrosis. For lung transplant patients, the risk of organ failure and death remains high. About half of transplanted lungs are still functioning five years after transplantation, according to the U.S. Organ Procurement and Transplantation Network.
A major limiting factor for long-term survival after lung transplant is graft rejection.
Research from the Department of Surgery at Washington University School of Medicine in St. Louis shows that a protein called IL-22 leads to the formation of tissues that are important for lung transplant tolerance. The research was published in the American Journal of Transplantation last year.
This June, members of the research team behind the study received the 2021 AJT Outstanding Article Award. Satona Tanaka, MD, Jason Gauthier, MD, and Daniel Kreisel, MD, PhD, received the award at the 2021 American Transplant Congress.
“This is a prestigious award in transplantation and a great recognition,” says Kreisel, who is surgical director of lung transplantation at the School of Medicine and Barnes-Jewish Hospital.
Kreisel, the G. Alexander Patterson, MD/Mid-America Transplant Endowed Distinguished Chair in Lung Transplantation, is principal investigator of two National Institutes of Health grants totaling $10 million to study how immune cells contribute to organ rejection, with the aim of improving the viability of organs after transplant.
Tanaka, a thoracic surgeon at Kyoto University in Japan, was a research fellow in the Kreisel Lab during the study.
Gauthier, who is first author on the article alongside Tanaka, is a general surgery resident at the School of Medicine.
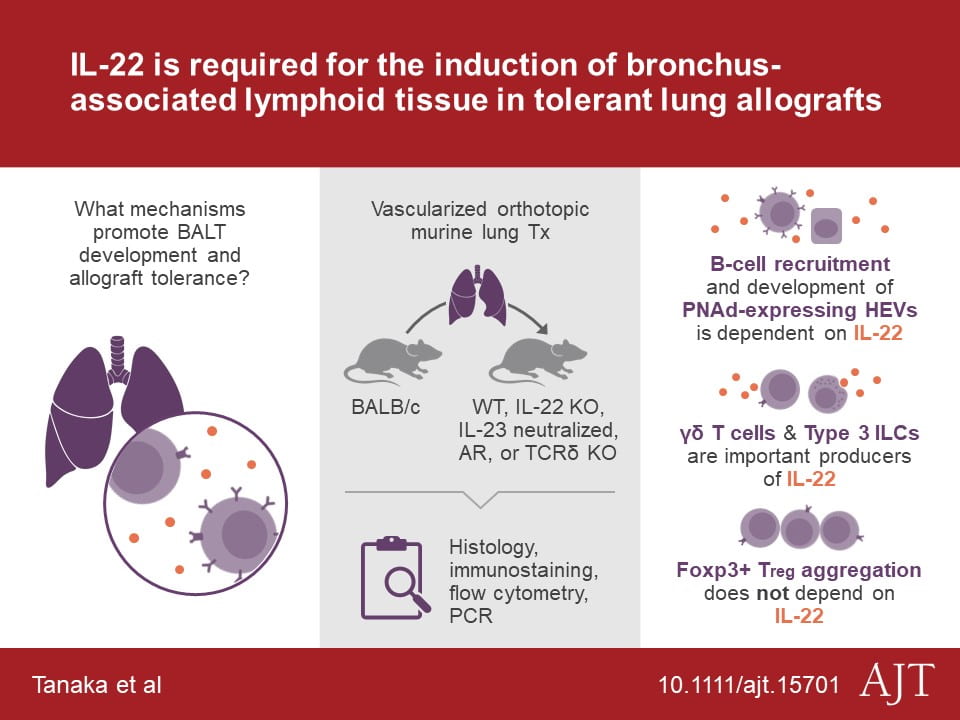
“Our study shows that IL-22 leads to the formation of bronchus‐associated lymphoid tissue, which we have previously shown to be important for lung transplant tolerance,” says Gauthier. “These findings identified novel cellular and molecular pathways following lung transplantation that may provide a platform for the development of new therapeutics.”
The study included surgeons and investigators from the Division of Cardiothoracic Surgery, Section of Acute and Critical Care Surgery, Department of Medicine and Department of Pathology & Immunology at the School of Medicine, as well as national and international medical centers.
Washington University lung transplant surgeons at Barnes-Jewish Hospital have performed over 1,800 transplants since the program began in 1988. The lung transplant program has survival rates above national averages, wait times shorter than the national average and a comprehensive, team-based approach to care throughout the transplant process. Innovative research, such as the AJT Award-winning study, aims to advance lung transplantation and improve transplant tolerance and patient outcomes.
