Hirschsprung disease, also referred to as congenital aganglionic megacolon, is a condition that occurs when a baby’s intestinal nerve cells (or ganglion cells) don’t properly develop. This change in development causes structural changes that then impact the effectiveness of the intestines. The progression of stool through the intestines is delayed, and the bowel becomes blocked with stool, causing chronic constipation. Complications can result in problems like diarrhea or severe infection. To avoid the long-term effects of Hirschsprung disease (HD), surgical treatment is required and lifestyle changes are recommended. Baddr Shakhsheer, MD, from the Division of Pediatric Surgery at the Washington University School of Medicine explains how this condition manifests, is diagnosed and is successfully treated.
What is Hirschsprung disease?
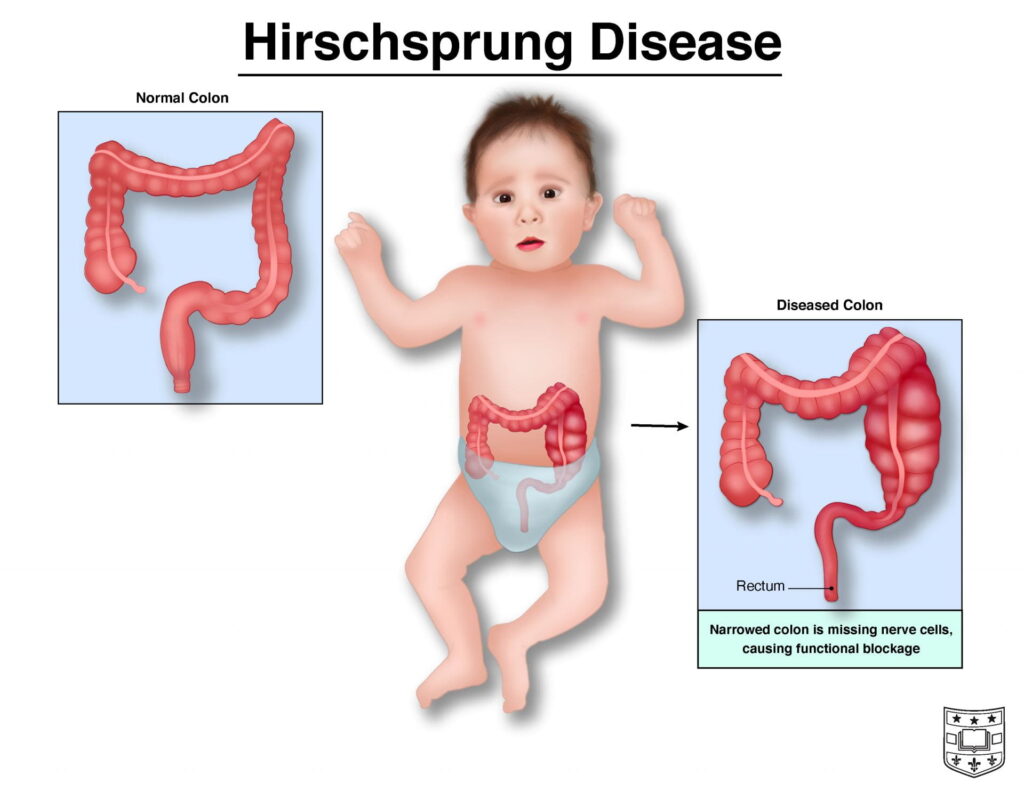
Hirschsprung disease (HD) is a condition usually affecting the large intestine or colon that impacts the passage of stool as it is expelled from the body. The colon contains many nerve cells that are responsible for the movement of stool. In a healthy colon, bowel movement is promoted by intestinal contractions and occurs without complication. In those affected by HD, this natural process is delayed and results in constipation because the bowel is missing these integral nerve cells. This condition manifests at birth and is considered a birth defect of the digestive system.
The most common areas impacted by HD are the sigmoid colon and rectum within the bowel, but some children are missing the nerve cells throughout their colon or even the small intestine. These different conditions are referred to as “short-segment Hirschsprung disease” and “long-segment Hirschsprung disease” respectively.

What causes Hirschsprung disease?
Hirschsprung disease manifests before birth. In early fetal development, nerve cells start at the beginning of the bowel and grow toward the end. In HD, these cells stop growing and do not reach the end of a child’s bowel, where the colon and rectum are located. This deficiency in cells means the bowel cannot contract sufficiently and thus delays the passage of stool.
The direct cause of HD disease is not known, and doctors aren’t sure why the necessary ganglion cells don’t migrate through the entire digestive tract. The condition appears to be an inherited congenital condition, meaning it occurs in families with some consistency. Genetic mutations may also cause this condition.
Are there risk factors that increase the chance of occurrence?
Because HD is related to genetics, there is an increased chance a child will have the condition if one of the parents does. In a family with one child who has Hirschsprung’s disease, there is a 3-12% chance that another baby from the same parents will have the condition. HD occurs in approximately one in 5,000 newborns.
HD occurs five times more often in biological males. Individuals with Down syndrome or congenital heart defects have a higher risk of having this condition, because HD is associated with some other inherited conditions. Those with Down syndrome have a one in 100 chance of having Hirschsprung.
What are the symptoms of Hirschsprung disease?
Symptoms of HD vary with its severity and usually appear shortly after birth, but it is possible the signs won’t be apparent until later in life. The most obvious sign of Hirschsprung is the inability of a newborn to have their first bowel movement within two days of birth. These babies also typically do not respond to constipation medicines meant to remedy digestive problems experienced by some newborns without Hirschsprung.
Other symptoms include:
- Swollen belly
- Vomiting
- Constipation
- Diarrhea
- Gas
- Fever
Any or all of these symptoms will usually be accompanied by excessive fussiness in the baby, related to the discomfort experienced during these issues.
If the condition is not diagnosed until later in life, older children may exhibit:
- Chronic constipation and gassiness
- Fatigue
- Growth delays
- Failure to thrive
Are there complications to Hirschsprung disease?
Children who have HD are more likely to develop a serious intestinal infection called enterocolitis. This infection causes fever, pain and diarrhea. Enterocolitis requires immediate treatment, because it can be life-threatening.
How is Hirschsprung disease diagnosed? When is the condition first detected?
Although the disease is congenital, no genetic testing exists to diagnose a child before birth. Because the condition is present at birth, detection is usually early. In milder cases, however, Hirschsprung might not be detected until later in childhood or even in adults.
A doctor will diagnose HD based on a physical exam, the medical history of the patient and their family, symptom presentation, and test results. Tests for HD include a rectal biopsy (in which a tissue sample is taken for examination), abdominal or lower intestine x-ray, or an anorectal manometry, which tests for contraction activity.
What surgical treatments are available? How does this improve quality of life?
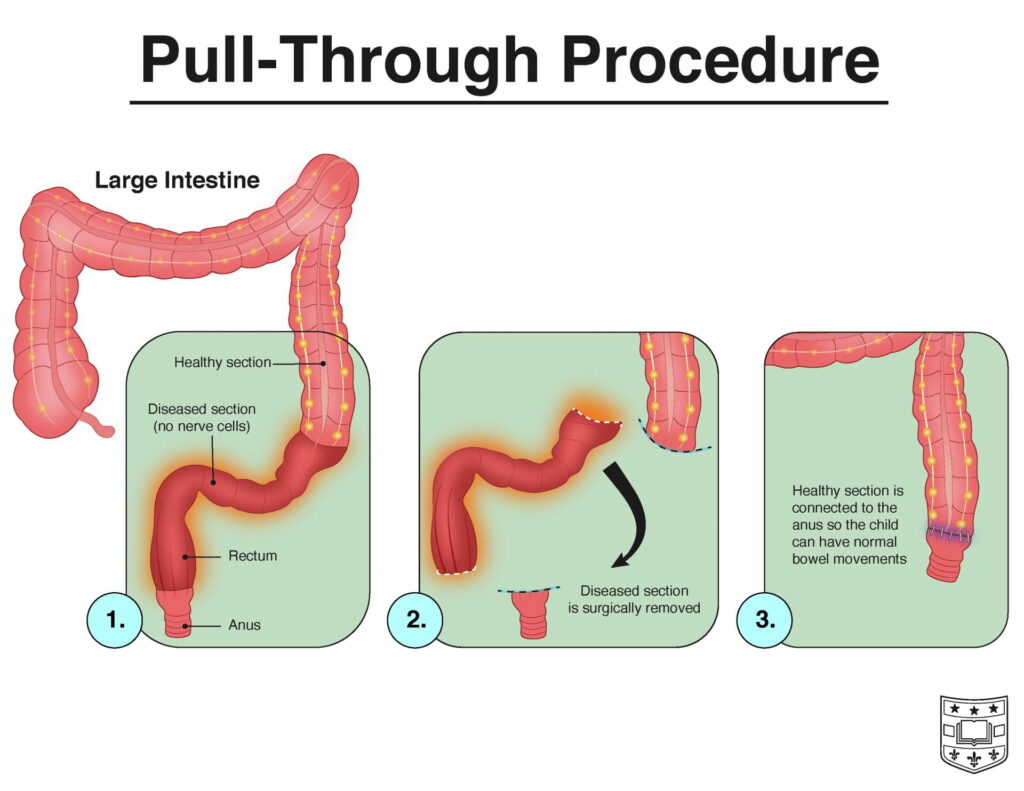
Surgery to bypass or remove the effected part of the colon is necessary for the patient to have proper bowel movements. Several options exist for surgical treatment of HD.
A pull-through surgery removes the diseased part of the colon or bowel. The section with nerve cells is then pulled through the colon and replaces the lost area. This procedure is done with minimally invasive (laparoscopic) techniques.
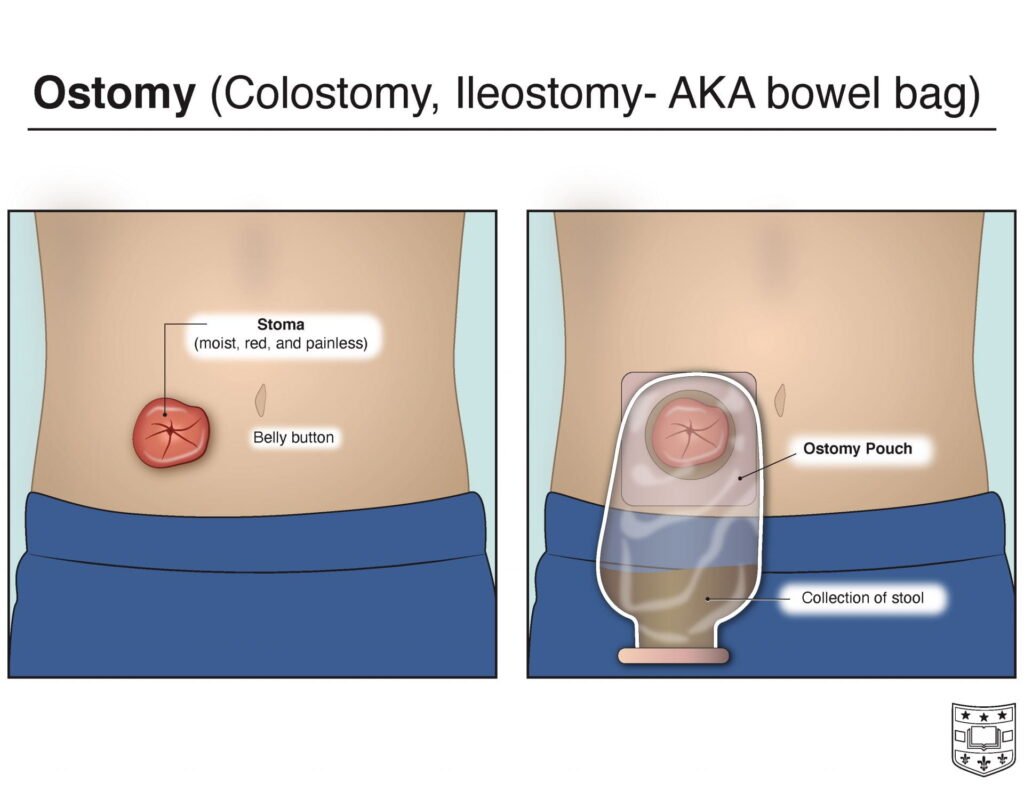
Ostomy surgery is an additional first step in very sick patients who cannot yet have the pull-through procedure. The ostomy method removes the abnormal portion of the colon while the healthy colon is routed to a surgical opening or “stoma” on the abdomen. Ostomy pouches are then attached to this abdominal port from which the stool is passed, collected and emptied. Once the colon has had time to heal in this position, the stoma is closed and the pull-through procedure is completed. If severe damage has occurred due to inflammation, the ostomy pouch system may be a permanent solution to prevent further damage.
How can lifestyle changes improve this condition? What are diet recommendations for someone with or recovering from Hirschsprung disease?
After surgery, it is still important to establish protocol in diet and activity to promote a healthy digestive system during recovery and throughout life for those effected by HD. For infants, this includes formulas to relieve constipation, increased fluids and laxatives as directed by a physician. For young children through adults, including high-fiber foods and physical activity will promote regular bowel movements.
Diet during recovery should consist of mostly liquid and soft foods, especially for infants and toddlers. A higher salt content in the diet is also necessary. Some infants may need feeding tubes for a short period.
Long-term dietary recommendations include high fiber and fluid intake. Food groups of choice are fruits and vegetables as well as fiber-enhanced cereals or grains. Low fiber foods like white bread are discouraged, as these can contribute to constipation.
Hirschsprung Treatment at Washington University

Treatment for Hirschsprung disease is essential for a healthy, comfortable life. Infants and children who undergo these procedures often find relief from the discomfort and complications caused by this condition.
Surgeons like Dr. Shakhsheer and others at the Division of Pediatric Surgery diagnose and treat patients from birth and older who require medical attention for HD. After surgery, the patient should follow up with a gastroenterologist to help address chronic issues related to HD.
The Pediatric Colorectal Center addresses the treatment of HD and more in young patients. Washington University Pediatric Colorectal Surgeons provide high-quality care to children with complex colorectal issues, including Hirschsprung disease, anorectal malformations, and severe chronic constipation.