Diabetes and peripheral vascular disease are two conditions known to cause foot complications including neuropathy, calluses, ulcers and poor circulation. These complications, described in detail by the American Diabetes Association, are difficult to treat because of the anatomy and dynamic weight-bearing surface of the foot. In the most severe cases, complications can lead to foot or leg amputation.
The alternative to amputation is “limb salvage,” a term used to describe surgery performed to save the form and function of a limb.
Surgeons from Washington University School of Medicine in St. Louis are expanding the possibilities for foot salvage surgery at Barnes-Jewish Hospital. John Felder, MD, Assistant Professor in the Division of Plastic and Reconstructive Surgery, describes one of these limb-saving procedures, called selective arterialization, in a recent journal article published in Plastic and Reconstructive Surgery—Global Open.
Going with the Flow
“In patients with peripheral arterial disease, the arteries of the leg progressively become occluded with plaque,” Felder illustrates. “Basically, the inside of the vessel fills up with chalk, so there is no more room in the tube for blood to get through.”
As more arteries fill up with this chalk-like plaque, less blood reaches the foot. For patients with diabetes and other vascular diseases, this reduced circulation makes it more difficult for soft tissue wounds to heal. To address this reduced blood flow, one limb salvage option is a bypass, connecting a vessel from above the occluded area to the foot. Vascular surgeons can perform this bypass if there are enough large, healthy vessels in the patient’s foot to circulate blood from the bypass vessel.

“However, if all of the small arteries of the foot have been filled up with plaque,” Felder says, “then even doing a bypass to a major artery at the ankle will not get blood up to the forefoot and toes where it is needed to heal the wound.”
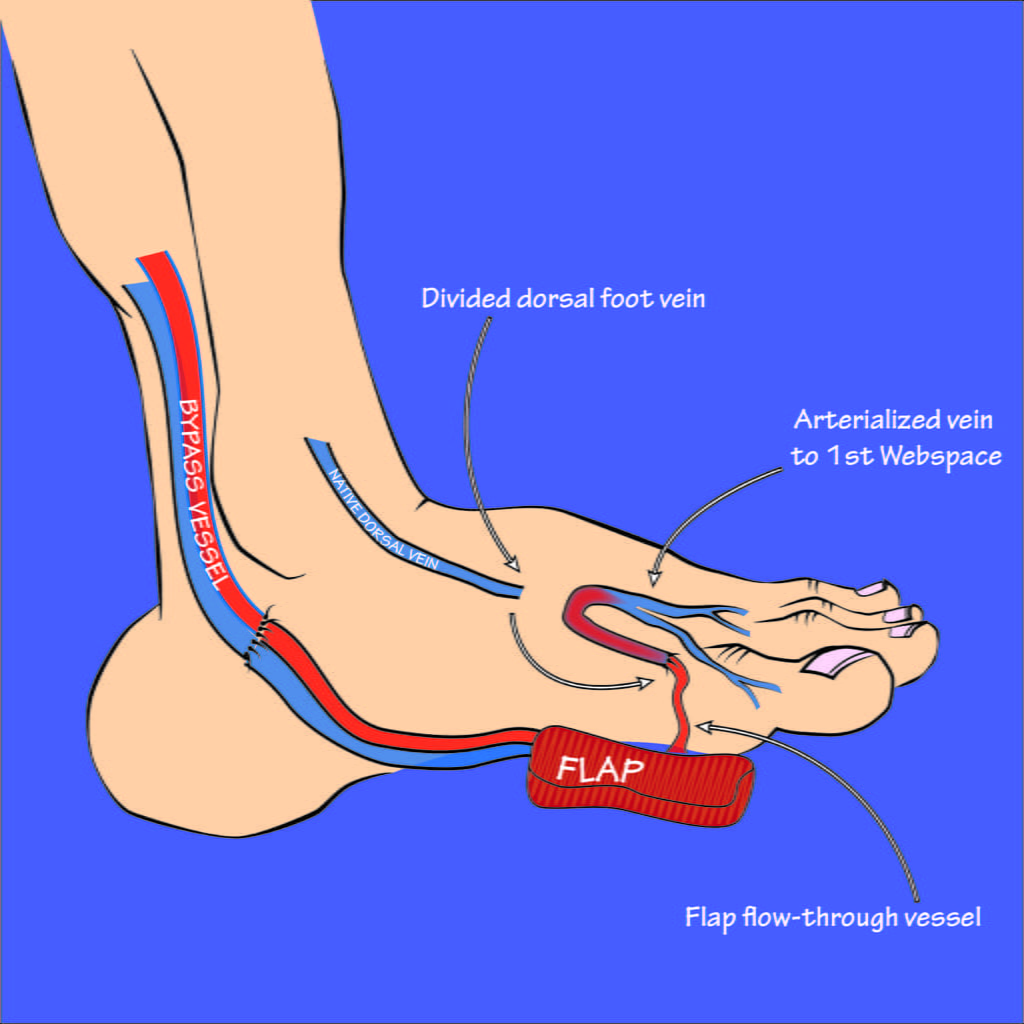
When this kind of bypass is not viable, surgeons have another limb salvage option: arterialization. Felder describes arterialization as converting veins into arteries. This conversion works by routing blood flow from an artery into the veins of the foot. Because veins do not tend to become occluded by peripheral vascular disease, blood is able to flow through them more regularly.
“The veins are just sitting there, open and healthy, but not adding any blood flow to the wound area, since veins only return blood to the heart,” Felder states. “So, by hooking up arterial blood flow into a vein, you are basically reversing flow in the veins and converting them into arteries that deliver oxygenated blood to where it is needed.”
The process of arterialization is not entirely new. Surgeons have used arterialization in limb salvage operations in the past, but these procedures have mostly been “global,” meaning that all of the veins in the foot were arterialized.
This is where the idea of selective arterialization originates. Working with a team of vascular surgeons including Patrick J. Geraghty, MD, John Ohman, MD, and Gerald R. Fortuna, MD, from the Section of Vascular Surgery, Felder has developed a form of arterialization that is targeted to a specific area of the foot that requires improved blood flow. For patients with wounds of the forefoot and toes, this more targeted approach may help them heal with fewer anatomical changes and less swelling than global arterialization.
Two Birds, One Stone
Felder became involved with limb salvage because of the need for multidisciplinary, team based care for patients with foot complications. In these cases, the patients often have soft tissue wounds that require reconstruction—Felder’s specialty.
With arterialization, patients may also require reconstructive surgery to cover a wound, such as an ulcer, that would not otherwise heal. This surgery can involve taking tissue from elsewhere in the body—what is called a “flow-through free flap”—and using it to cover the wound. In cases requiring both a flow-through free flap and selective arterialization, it is possible to use a free flap containing blood vessels that can then be arterialized.
“In cases like this, you need to cover the wound with healthy tissue, and you also need to provide more blood flow and nourishment to the tissue around the wound so it will heal and remain healthy,” Felder says. “Instead of using a separate bypass graft to accomplish this, we can use the blood vessels that come with the free flap. Doing this allows us to accomplish two goals with one piece of tissue. We can address two birds with one stone, so to speak.”
Felder and his colleagues in Plastic and Reconstructive Surgery and Vascular Surgery are developing a growing limb salvage service at Barnes-Jewish Hospital, in hopes that they can reach more patients for whom limb salvage is a better outcome than amputation.
Reconstructive foot surgery is difficult and involves a long recovery process of at least eight weeks. Felder cautions that, for particularly complex procedures, such as the selective arterialization with a flow-through free flap, recovery time might be closer to three months, including two weeks in the hospital postoperatively.
Selective arterialization is a newer form of limb salvage, which Felder intends to study further. Felder sees limb salvage as a specialization with great room for innovation. “Patients with these complications have been historically underserved,” Felder recognizes. “But serving these patients is very gratifying, and we have the experts here to provide comprehensive care.”
As innovation and infrastructure continue to grow around this developing limb salvage service, the plastic and reconstructive and vascular surgeons of Washington University will continue to offer comprehensive care to patients needing limb salvage operations.
“At Washington University, we have the rare but fortunate circumstance of having both the vascular surgeons and the plastic surgeons that possess the skills and interest needed to form this type of team,” Felder states. “When colleagues come together, each bringing their own expert tool belt, the options for how to accomplish your goals suddenly expand.”
