Plastic and reconstructive surgery is a truly head to toe specialty. From craniofacial surgery for adults and children to operations that help people avoid foot and leg amputations, plastic and reconstructive surgeons at Washington University School of Medicine in St. Louis treat conditions affecting every part of the body.
They also see themselves as problem-solvers. Plastic and reconstructive surgeons and investigators at the School of Medicine advance the field and improve patient care through their research in the Plastic Surgery Research Laboratories (PSRL). The PSRL are a consortium of investigators in plastic and reconstructive surgery with a common objective of investigating the pathology, mechanisms and prospective clinical treatments for the problems still facing plastic and reconstructive surgeons.
Led by Scientific Director Matthew Wood, PhD, the laboratory contains over 2,000 square feet of lab space and has the research infrastructure to perform the highest level of basic science investigation in tissue engineering, immunology and nerve physiology.
“It is an exciting time to be part of the Division of Plastic and Reconstructive Surgery,” says Division Chief Justin Sacks, MD, MBA, the Shoenberg Professor of Plastic and Reconstructive Surgery. “We are growing our research programs to complement all of the division’s clinical programs. This institution is a powerhouse of plastic surgery research.”
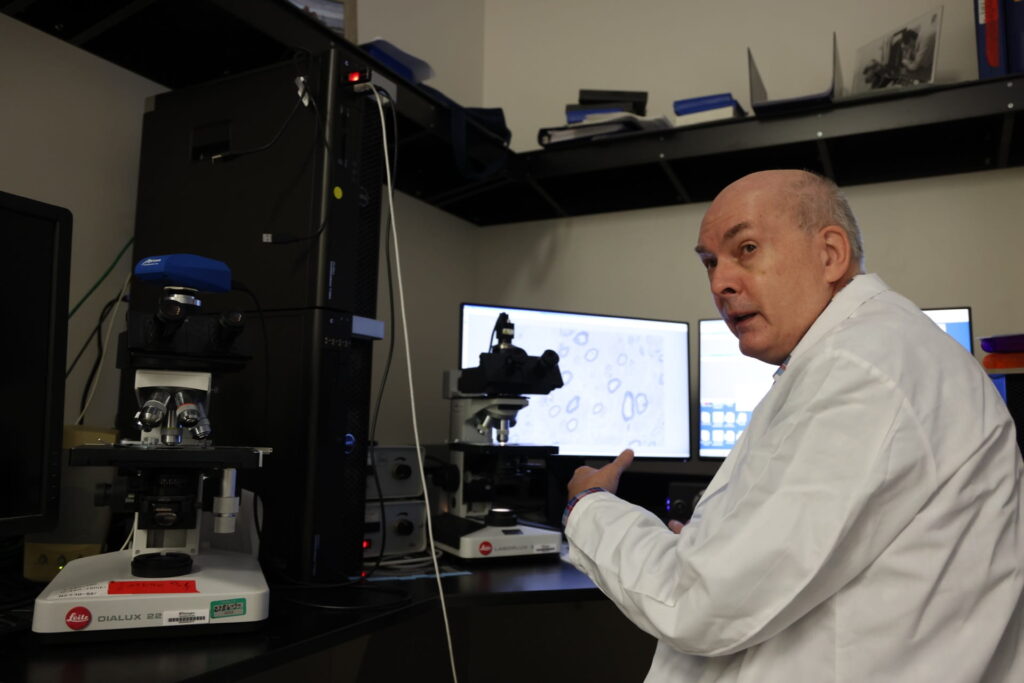
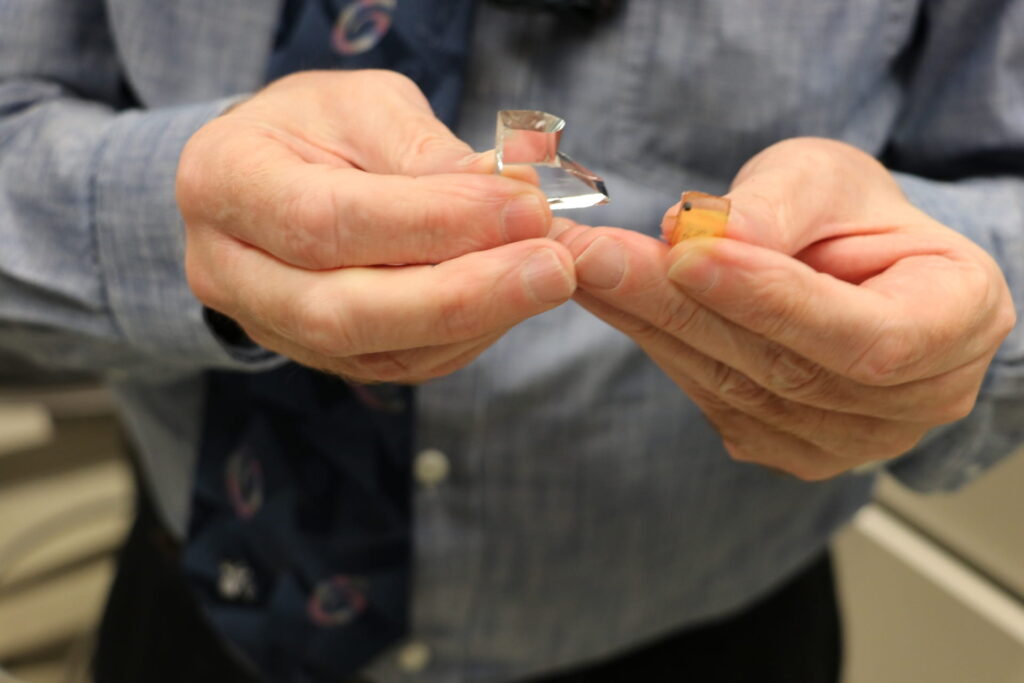
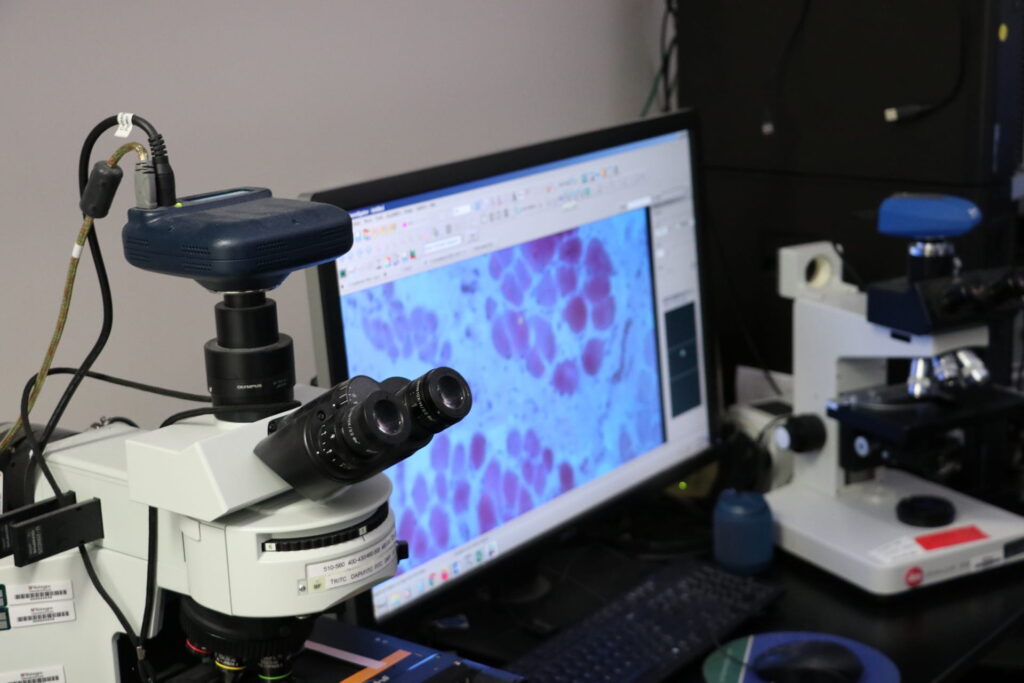
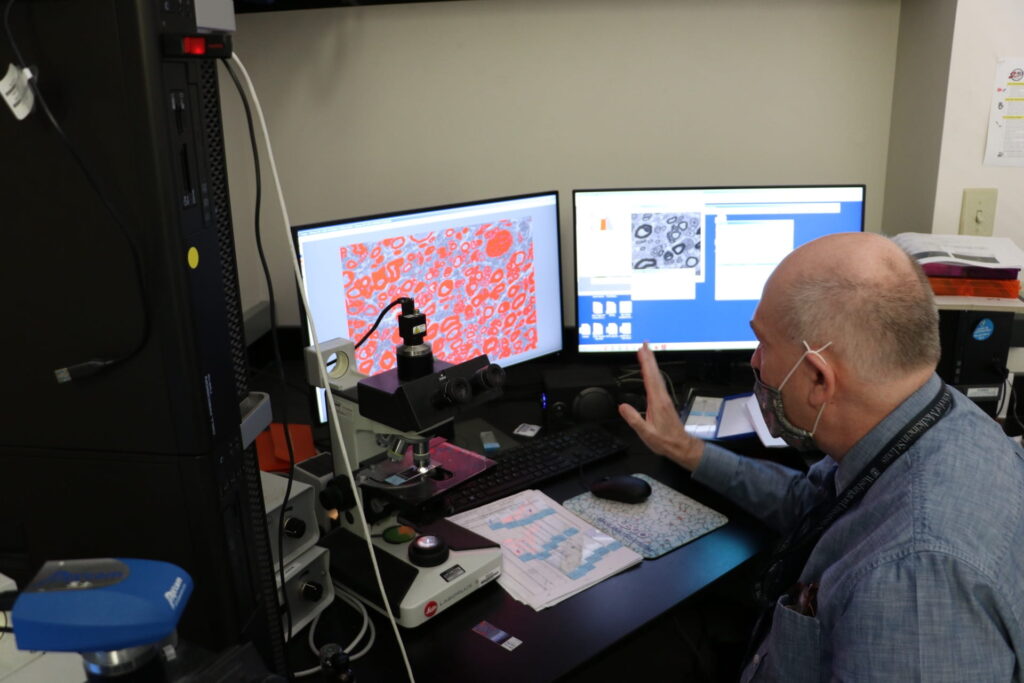
Past research has led to advances and breakthroughs in peripheral nerve surgery at the medical school. Senior scientist Dan Hunter has developed methods of precisely counting and measuring nerve fibers. These techniques—which blend new technology and what Hunter calls “old fashioned” methods—have helped clinicians and researchers quantitatively understand nerve injury and recovery.
“People used to count nerve fibers by hand. This was tedious and took a lot of time,” Hunter recalls. In 1989, Hunter wrote a software program to analyze nerve fibers more effectively and efficiently. Now it is possible to precisely measure nerve regeneration or degeneration at a microscopic level. Hunter says that paradigm shifts in technology and techniques have helped PSRL researchers remain national and international leaders in their fields of study. “You’re not just showing a pretty picture. You can back it up with data.”
Hunter is eager to see the PSRL expand to address problems facing plastic and reconstructive surgeons across all clinical programs.
“Very few labs have the equipment and capabilities we have at Washington University,” Hunter says. “What does that mean for our lab? We can use what we have to explore research problems in every area of plastic surgery.”
The Division of Plastic and Reconstructive Surgery has 10 core clinical programs:
- Aesthetic surgery
- Breast surgery
- Adult craniofacial
- Pediatric plastic surgery
- General reconstructive surgery
- Hand surgery
- Limb preservation
- Lymphedema surgery
- Nerve surgery
- Gender affirming surgery
Research projects in the PSRL go from bench to bedside to help patients in each of these programs.
A Research Powerhouse
This year marks the 30th anniversary of the PSRL at the School of Medicine.
Established in 1991 by Susan Mackinnon, MD, the Minot Packer Fryer Chair of Plastic Surgery, the laboratory has long been an international leader in nerve research. Mackinnon performed the first ever human nerve transplant in 1988, using nerves from a cadaver to restore movement and feeling to a boy’s injured leg. In the years since, Mackinnon and the team of investigators in the laboratories have pioneered a new era of nerve surgery, developing advanced techniques and a greater understanding of nerve injury and regeneration.
The laboratory continues its legacy as a powerhouse of peripheral nerve research. Last year, Hunter and Wood, who are investigating the role of T cells in nerve injury and regeneration, published a book chapter on the role of histologic analysis in neuroma pathology. The team’s research has contributed to a deeper understanding of neuroma—a painful growth of nerve cells at the site of a nerve injury. PSRL researchers have been continuously NIH-funded since 1993, and have published more than 1,000 peer-reviewed articles and several dozen books and chapters.
“As part of our effort to think about problems in plastic surgery in ways that others have not, we are recruiting and building a team for diverse ideas,” says Wood. “We have new team members that will help us growth research programs to complement our core clinical programs.”
This June, Xiaowei Li, PhD, joins the laboratory as assistant professor of surgery in the Division of Plastic and Reconstructive Surgery. Li is an expert in bioengineering strategies for tissue engineering. Li and Sacks worked closely together at Johns Hopkins School of Medicine, where they collaborated on research focused on soft tissue regeneration.
“The arrival of Dr. Li marks an exciting period of growth for the Plastic Surgery Research Laboratories,” Sacks says. “We are going to expand on what is already established and grow tissue engineering and biomedical innovation as new areas of excellence.”