The Extracorporeal Membrane Oxygenation (ECMO) Program at Washington University (WU), in partnership with Barnes-Jewish Hospital (BJH), provides lifesaving support to people with life-threatening heart and lung conditions. ECMO, sometimes called extracorporeal life support (ECLS), temporarily takes over for the heart, lungs, or both, when they are not working properly.
ECMO works like an artificial heart and lung. The ECMO machine removes blood from the body through large tubes, called cannulas. The blood is pumped through a filter, which removes the carbon dioxide and puts oxygen into the blood. Once the blood is enriched with oxygen, the ECMO machine pumps the blood back into the body.
ECMO is used as a bridge therapy. This means it does not cure the underlying condition that caused the heart or lungs to stop working. Instead, it gives the body time to heal before another type of treatment. Depending on your condition, ECMO may be used for a few days or several weeks.

Proud to be named an ELSO Silver Level Center on the Path to Excellence in Extra Corporeal Life Support. The Excellence in Life Support Award recognizes those centers that demonstrate an exceptional commitment to evidence-based processes and quality measures, staff training and continuing education, patient satisfaction and ongoing clinical care. Washington University, in partnership with Barnes Jewish Hospital is the only Adult ECLS center in Missouri to receive the Excellence in Life Support Award for the Award Period 2023-2025
Contact us
If you need to transfer a patient to Barnes-Jewish Hospital please call the BJC Transfer Center at 800-252-DOCS (3627). Our trained specialists will help you find the best care for your patient
FOR REFERRING PHYSICIANS
When to contact
There are no standard criteria for transfer.
The referring physician should begin to consider the need for ECMO when a patient who has received appropriate medical management has a Pa02 of 50-60 mm Hg when the PIP is >35 cmH20 and the FI02 is 100% on optimized conventional ventilation, considering prone positioning, or high inotropic/ vasopressor support.
Early consultation with the ECMO team will allow the referring physician peace of mind that support is available. This will also allow for coordination of the safest time and route to transport the patient, bed planning logistics, and specialty team activation.
- Adult ECLS Inclusion criteria
- Cardiogenic Shock:
- Non-improving hemodynamic status
- Cardiac index <2.0 L/min/m2
- High dose single inotropic support
- More than one inotrope or pressor support
- Patient is best served before or as soon as developing signs of end organ malperfusion:
- Non-improving hemodynamic status
- Cardiogenic Shock:
- Signs of end-organ malperfusion
- Altered mental status due to brain hypoperfusion
- Worsening lactic acidosis (Increased lactate >3.0)
- Liver enzyme increase or signs of acute liver failure
- Acute oliguria or anuria with acute creatinine
- Respiratory Shock
- Severe hypoxemic (or mixed hypoxemic/hypercapnic) respiratory failure despite ventilator optimization and use of adjunctive ARDS therapies
- PF ratio of <100 for >3 hours
- pH <7.25, PCO2 >60, PaO2 <60
- Plateau pressure >25, PEEP >10, peak pressure >40
- Acute severe asthma with persistent pH <7.25 despite ventilator optimization, nebulization and steroids
- Advanced lung disease with active listing for lung transplantation, with input from lung transplant team
- Severe hypoxemic (or mixed hypoxemic/hypercapnic) respiratory failure despite ventilator optimization and use of adjunctive ARDS therapies
- Adult ECMO relative contraindications – each patient will be evaluated on a case-by-case basis
- Functional debility at baseline
- Advanced chronic lung disease (other than asthma) on home O2 without active listing for lung transplantation
- Prolonged period of mechanical ventilation (generally >7 days)
- Terminal cancer
- Irreversible or chronic cause of cardiac dysfunction
- Bleeding diathesis/hypocoagulability
- Long-term dialysis
- Major stroke
- DNR status
- BMI > 40
Multidisciplinary ECMO Care Team
ECMO is a complex therapy that requires expertise in several areas of patient care. During ECMO treatment, patients receive multidisciplinary care from an experienced team around the clock.
Cardiothoracic Surgeons

Amit A Pawale, MBBS, FRCS, FACS
Associate Professor of Surgery
Section of Cardiac Surgery
Division of Cardiothoracic Surgery

Kunal Kotkar, MD
Associate Professor of Surgery
- Phone: 314-362-7260
Section of Cardiac Surgery
Division of Cardiothoracic Surgery

Muhammad Faraz Masood, MD
Associate Professor of Surgery
- Phone: 314-362-7260
Section of Cardiac Surgery
Division of Cardiothoracic Surgery

Matthew R. Schill, MD
Assistant Professor of Surgery
Section of Cardiac Surgery
Division of Cardiothoracic Surgery

Nicole Schweiss
Acute Care Nurse Practitioner
Acute Care Nurse Practitioner
Advanced Practice Provider Leadership

Ellen Stemmler
Acute Care Nurse Practitioner
Acute Care Nurse Practitioner
Advanced Practice Provider Leadership

Samantha Miller, MSN, RN
Patient Care Director
Patient Care Director
Heart and Vascular Services
Barnes-Jewish Hospital
Our ECMO team collaborates with other specialists when needed to deliver the best possible care. Our partners sometimes include: Washington University Neurologists, Neurosurgeons, Cardiologists, Pulmonologists, Heart and Lung Transplant teams, Vascular surgeons, Nephrologists, Infectious Disease doctors, Hematologists, Maternal Fetal Medicine doctors, and Neonatologists.
Our team of Washington University Physicians provide ECMO support at Barnes-Jewish Hospital, the top-ranked hospital in St. Louis and Missouri, according to U.S. News & World Report. We lead one of the highest volume ECMO programs in the region. In recent years, our program has provided ECMO support to over 200 patients per year. This means that patients have access to an experienced, dedicated team of ECMO specialists.
ECMO at Washington University and Barnes-Jewish Hospital
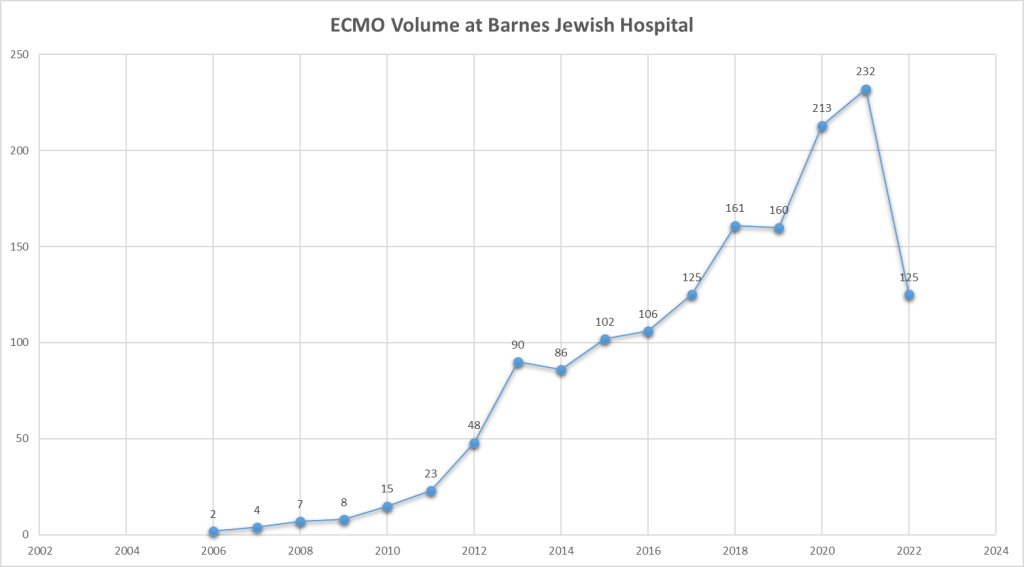
- 2006 First ECMO run. We now average over 150-200 runs per year.
- 2011 WU/BJH instituted the “Shock Service” to provide lifesaving support to community hospitals that need to partner for cardiogenic shock and advanced heart failure therapies.
- BJH first Heart Transplant: 1/10/1985
- BJH first Lung Transplant: 4/16/88
- BJH first LVAD: 1985
- BJH first percutaneous mechanical circulatory support: 6/12/2010
Indications for ECMO
ECMO is used to perform the functions of the lungs and heart when other life support therapy is not successful. This can happen after any major condition affecting the lungs or heart, including infections, chronic conditions, and traumatic injuries.
There are two major types of ECMO. One type, called V-V ECMO, takes over for the lungs when they cannot properly function. The other type, called V-A ECMO, can take over when the heart or the heart and lungs both cannot function properly.
2 Major Types of ECMO:
V-V ECMO (or veno-venous ECMO) bypasses the gas exchange to the patient’s lungs. It is used when the lungs are damaged and cannot remove carbon dioxide and introduce oxygen into the blood stream. Blood is removed from the body through a cannula, or tube, in a large neck or groin vein. Blood is pumped to a filter that removes carbon dioxide and enriches the blood with oxygen. The blood is then pumped back into the body through a cannula in a different vein.

Conditions that may require V-V ECMO support:
- Pneumonia or virus (Influenza or COVID-19)
- Pulmonary embolism
- Chronic Obstructive Pulmonary Disease (COPD)
- Asthma
- Cystic Fibrosis
- Pulmonary embolism
V-A ECMO (or veno-arterial ECMO) bypasses the body’s cardiopulmonary function. It is used when the heart or heart and lungs cannot effectively oxygenate and pump blood to the rest of your body. Blood is removed from the body through a cannula, or tube, in a large vein. Blood is pumped through the filter to remove carbon dioxide and enrich the blood with oxygen. Then the blood is pumped back into the body through a cannula placed in a large artery. The artery then carries oxygenated blood through the body.

Conditions that may require V-A ECMO:
- Major heart attack
- Inflammation of heart tissue due to virus or bacterial infection
- Drug overdose
- Post-partum cardiomyopathy
- Support after a heart or lung transplant
- Traumatic injury
Treatment
Every patient’s ECMO experience is unique. Our multidisciplinary team creates a plan of care individualized to each patient’s needs.
ECMO is a lifesaving and life-altering bridge treatment. It does not cure the underlying problem that caused the lungs or heart to fail. ECMO performs the work of the lungs and heart while the body heals. ECMO is typically used as a bridge to:
- Lung or heart recovery
- Left ventricular assist device (LVAD) implant
- Heart or lung transplant
- Other patient-focused treatment decisions
ECMO is a major life support treatment. We consider using ECMO when the risk of dying from heart or lung failure is very high. Timing of implementation of ECMO depends on each individual’s circumstances.

Rehab and Recovery
The road to rehabilitation and recovery after ECMO looks different for everyone. The rehab and recovery process will depend on the condition that necessitated ECMO.
Our team includes a Registered Dietician, who asses each patient’s needs daily to provide personalized nutritional support. Optimum nutrition during ECMO treatment helps maximize recovery.
Physical Therapy plays an important role in recovery from life-threatening heart and lung conditions. Our therapists and occupational therapists collaborate with experts from the intensive care unit to determine the safest mode of therapy for each ECMO patient. Therapy can vary from day to day, but typically includes, at a minimum, passive range of motion exercises and can progress to ambulation on the ECMO machine.
What to Expect
During ECMO treatment, patients will receive specialized care from a multidisciplinary team of physicians and nursing staff. Members of the ECMO, intensive care unit, and palliative teams assess each patient and review their status and care plan during daily rounds.
Frequent goals of care discussions are an important part of ECMO care. Our Palliative Care team provides comprehensive management of the physical, psychological, and spiritual issues related to a patient’s illness. ECMO can provide lifesaving support when a patient’s risk of dying from their heart and/or lung failure is greater than 80%. These patients are at high risk for complications inherent to severe illness. The addition of ECMO support can increase the risk. When on ECMO, your blood is taken out of your body.
Some of these risks include:
- Blood clots: When blood comes in contact with anything other than blood vessels, its natural reaction is to form a blood clot. This risk can be avoided by using intravenous blood thinners.
- Bleeding: Blood is pumped to the ECMO machine through a large cannula tube placed in a major blood vessel or artery. There can be bleeding from the cannula entry points. The blood thinners that prevent blood clots can cause increased bleeding risk. It is not uncommon for patients on ECMO to require blood transfusions.
- Stroke: This can be due to bleeding or blood clots in the brain that damages brain tissue.
- Infection: ECMO is placed under sterile procedures, but there is always a risk of infection. We monitor closely for signs and symptoms of infection and treat with antibiotics.
- Loss of blood flow to fingers, toes, hands or feet. This may result in the amputation of the area affected by the loss of blood flow.
- Malnutrition: The body needs nutrition to heal. Some people on ECMO require a small temporary feeding tube placed through the nose into the intestines so nutrition can be provided.
- Kidney injury: It is not uncommon for patients on ECMO to require dialysis. It is typically short term and no longer needed once the patient goes home. Dialysis treatment can require placement of another large IV in the patient’s neck or groin.
Location
You may contact the Division of Cardiothoracic Surgery at Washington University School of Medicine by writing or calling:
Campus Box 8234
660 S. Euclid Ave.
St. Louis, MO 63110









