The heart and lungs are vital organs that are always working to keep the body healthy. The air you breathe gets pumped through the body through the blood in your circulatory system. When something causes damage to the heart or lungs, they may not be able to do the work they need to keep you alive. This is called heart or lung failure.
During heart or lung failure, a kind of treatment called extracorporeal membrane oxygenation (ECMO) can take over until the heart or lungs are healthy enough to get back to work.
Washington University surgeons are part of a multidisciplinary team of experts who provide lifesaving ECMO support at Barnes-Jewish Hospital.
Healthy Lung and Heart Function
Normally, the heart and lungs work together to bring oxygen into the body and remove carbon dioxide. This process includes the blood pumping through your circulatory system, as well as the constant work of breathing in and out through your respiratory system.
Your lungs are the pair of spongy, pinkish-gray organs in your chest.
When you inhale (breathe in), air enters your lungs, and oxygen from that air moves to your blood. At the same time, carbon dioxide, a waste gas, moves from your blood to the lungs and is exhaled (breathed out). The lungs, windpipe, muscles of the chest wall and diaphragm, blood vessels and other tissues make up your respiratory system. Your brain controls how fast or slow you breathe by sensing your body’s need to get oxygen and remove carbon dioxide.
The heart is an organ about the size of your fist that pumps blood through your body.
The circulatory system carries blood, which contains the oxygen and nutrients your organs need, to and from all areas of your body. Blood also carries carbon dioxide to your lungs so you can breathe it out. Inside your heart, valves keep blood flowing in the right direction.
Oxygen-rich blood enters the left atrium of your heart and gets pumped to your whole body through your blood vessels. This oxygen is replaced with carbon dioxide. Then the oxygen-poor blood enters your heart through veins and is pumped back to your heart from your right ventricle.
Read more: How and Why to Donate Blood
Causes of Heart and Lung Failure
Most of the time, the heart and lungs work without any issue. Your brain tells your respiratory system to breathe, and your body’s electrical system keeps your heart beating. Sometimes, a problem can cause the heart, lungs or both organs to stop working properly.
Conditions that may lead to lung damage include:
- Traumatic injury: Lung injuries can happen during car accidents, falls, explosions or any other incident that causes trauma to the chest. These injuries can cause serious damage to the lungs.
- Pneumonia or virus: Infections like pneumonia, influenza (the flu) and COVID-19 can cause lung damage that may be serious and life-threatening.
- Chronic obstructive pulmonary disease (COPD): A chronic (long-term) inflammatory lung disease that causes blocked airflow from the lungs.
- Asthma: A chronic condition that causes difficulty breathing, chest pain, cough and wheezing. Severe cases may lead to serious lung damage.
- Cystic fibrosis: An inherited disorder that can cause lung infections and damage the lungs.
- Pulmonary embolism: A blood clot that blocks blood flow in the lung.
Conditions that may lead to heart damage include:
- Major heart attack: A blockage of blood flow to the heart.
- Inflammation of heart tissue: Swelling caused by your body’s reaction to a virus or bacterial infection.
- Traumatic injury: Heart injuries can happen during car accidents, falls, crush injuries, sports-related injuries, stabbings, gunshot wounds or any other incident that causes trauma to the chest.
- Drug overdose: An overdose of opioids, prescription drugs including heart medicines, and harmful substances can cause damage to the heart.
- Post-partum cardiomyopathy: This uncommon form of heart failure happens during the last month of pregnancy or in the months after giving birth. The heart chambers enlarge and the muscle weakens, leading to decreased blood flow.
When one of these conditions or another severe problem causes heart or lung failure, ECMO may be a life-saving option to help support the body.
How ECMO Works
ECMO uses mechanical devices to replace the function of the heart and lungs when they stop working. This allows the heart and lungs to rest while your body still gets the healthy, oxygenated blood it needs.
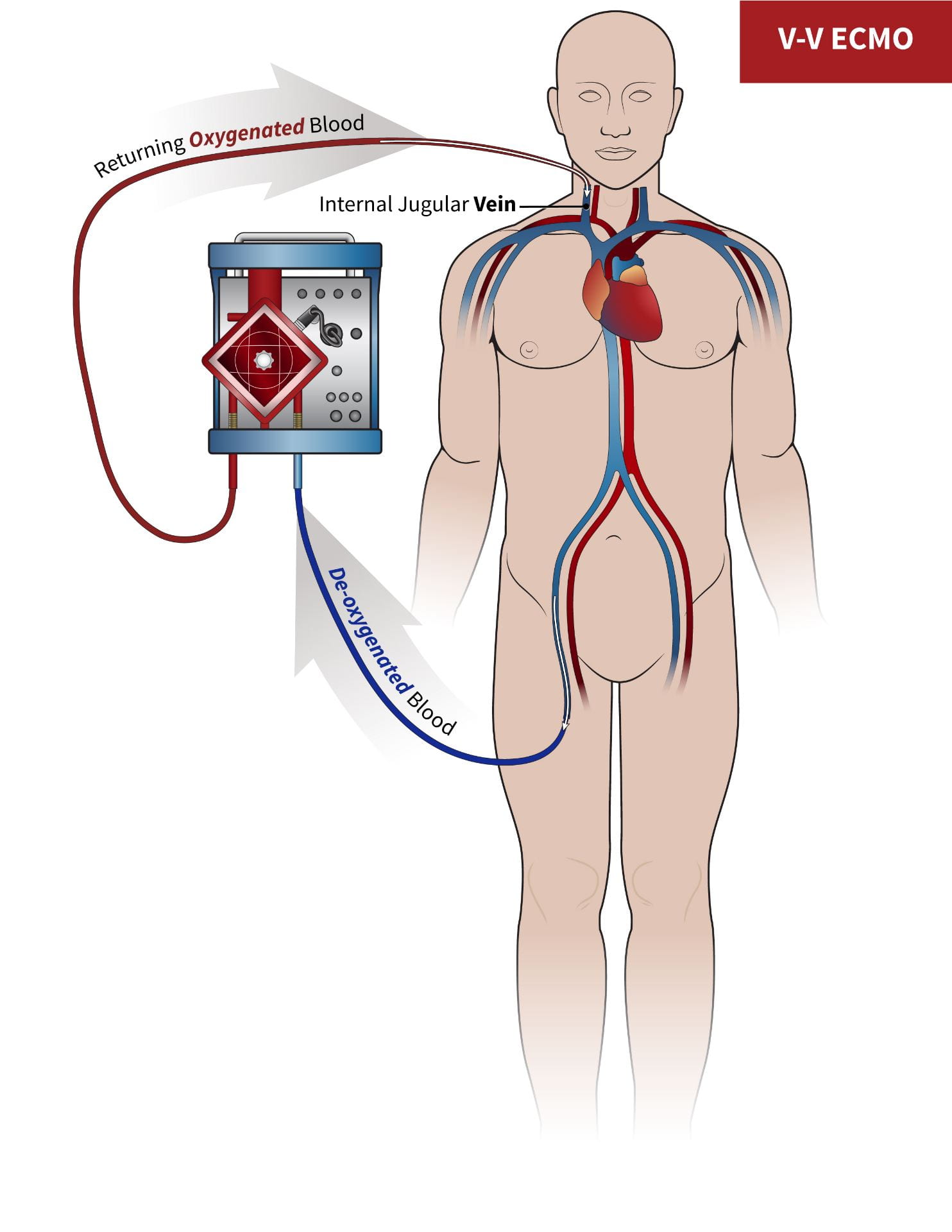
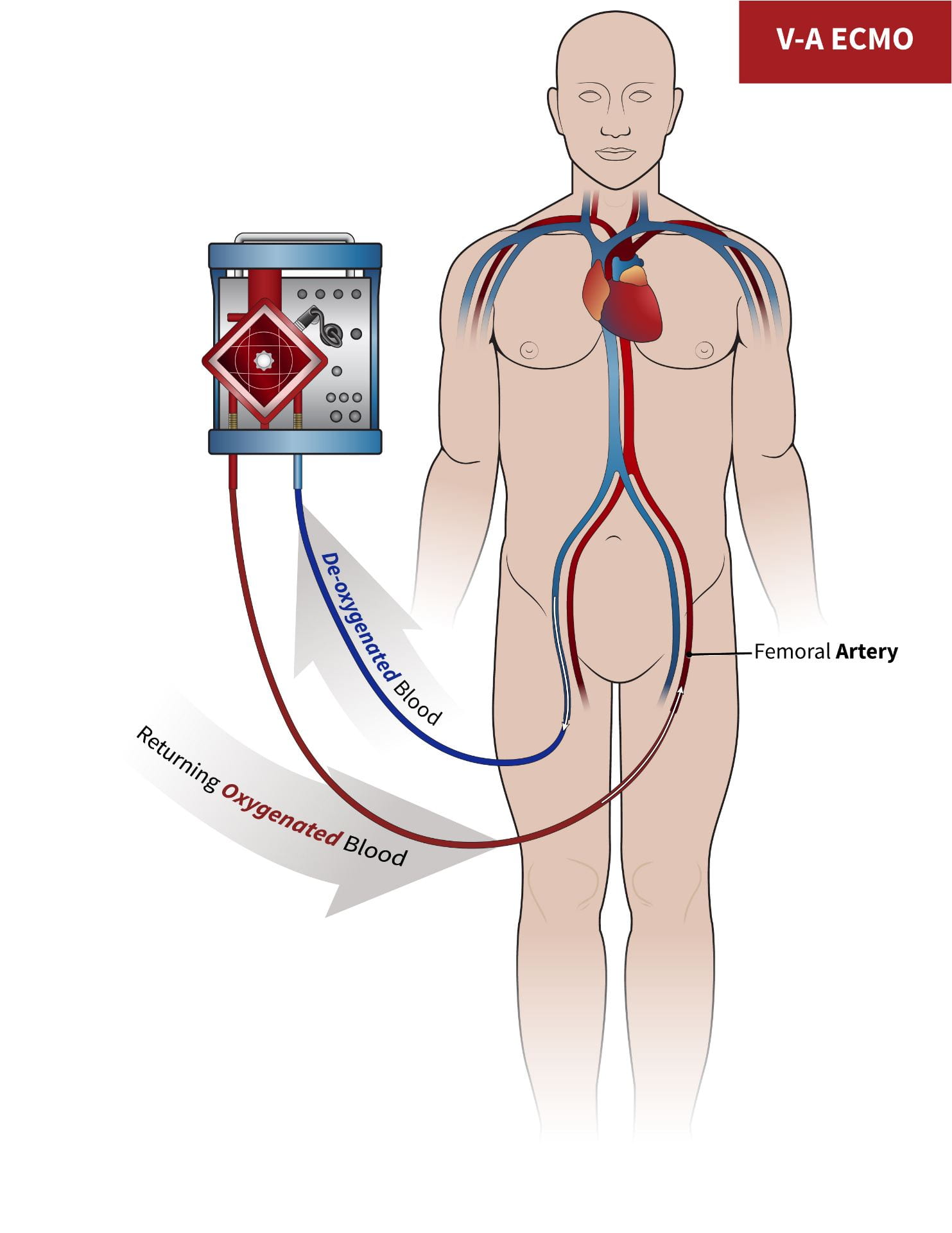
The ECMO machine pumps blood out of the body through a large tube called a cannula. This cannula carries the blood to a filter, which pumps out the carbon dioxide and pumps oxygen into the blood. The oxygenated blood then gets pumped back into your body through another cannula tube.
There are two main types of ECMO:
- V-V ECMO: Veno-venous ECMO, or V-V ECMO, bypasses the lungs. The machine is connected to your veins and is used when there is a problem with only the lungs.
- V-A ECMO: Veno-arterial ECMO, or V-A ECMO, bypasses the heart and lungs. The machine is connected to a vein and an artery and is used when there is a problem with both the heart and lungs.
ECMO can also provide support after a heart or lung transplant. When you have an organ transplant, it may take time for your body to start working properly again. During that time, ECMO can replace the function of your heart or lungs, reducing the amount of work your body needs to do at first.
What to Expect After ECMO
ECMO is considered a “bridge” therapy. This means that ECMO does not treat the condition that caused heart or lung problems. Instead, ECMO allows your body to rest. Depending on the problem that led to heart or lung failure, the body may recover while on ECMO, or you may need another kind of surgery or treatment.
ECMO gives your care team the time they need to provide the best possible care for your condition. Your doctors will work with you and your family to develop the right plan for your care during and after ECMO treatment.
The Washington University ECMO Program
The Washington University ECMO Program provides lifesaving support to people with heart and lung conditions. Our team of Washington University Physicians provide ECMO support at Barnes-Jewish Hospital, the top-ranked hospital in St. Louis and Missouri, according to U.S. News & World Report.
The ECMO care team includes expert surgeons, nurses, critical care doctors and other specialists. Together, our team provides ECMO support for over 200 patients per year, one of the highest volumes in the region.
To learn more about the Washington University ECMO program, please visit our website.
To transfer a patient to Barnes-Jewish Hospital please call the BJC Transfer Center at 800-252-DOCS (3627). Our trained specialists will help you find the best care for your patient.