General surgery residents at Washington University School of Medicine in St. Louis receive surgical training in one of the nation’s top programs, preparing them for careers as leaders in their specialties. This May, two residents paid it forward by joining a surgical mission trip to El Salvador. The mission trip, led by the nonprofit organization Surgical Outreach for the Americas (SOfA), delivered quality surgical care to communities lacking medical resources at no cost to the patients.
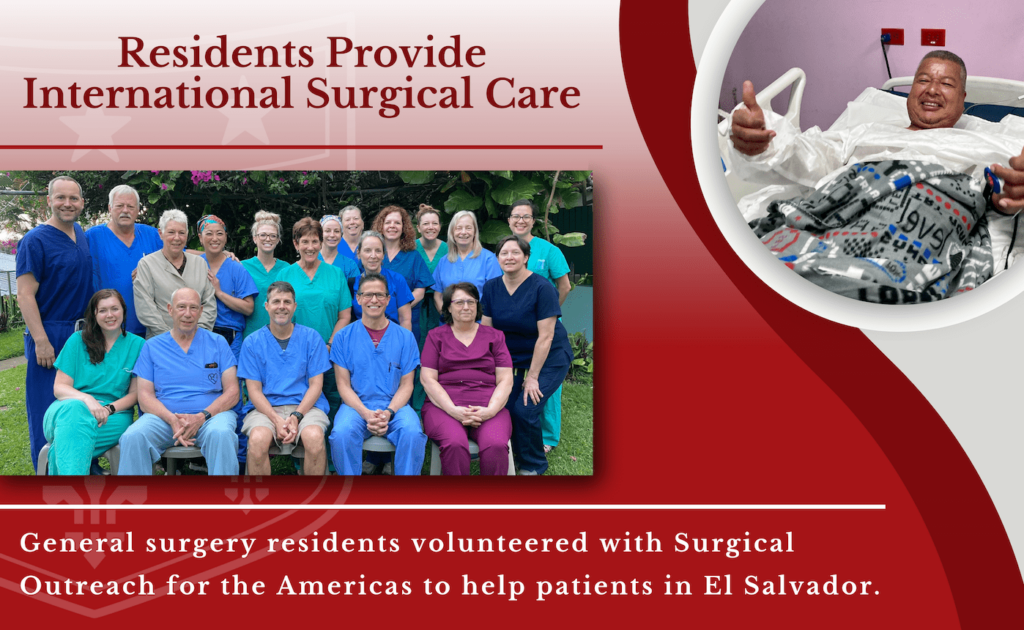
During the weeklong mission, general surgery residents Hailey Shepherd, MD, and Meghan Kelly, MD, saw numerous patients at a local hospital in Texacuangos, El Salvador. Shepherd and Kelly were joined by general surgeons and pediatric surgeons, anesthesiologists and certified registered nurse anesthetists (CRNAs), gynecologists, nurses and translators. In total, the team performed 99 surgeries and saw roughly 150 patients.
“One of the most rewarding parts of this trip, for me, was having the ability to care for patients without any of the distractions which can detract from that simple—but not easy—and certainly most important, part of my job: taking care of people,” Kelly says.
Both Kelly and Shepherd learned from the experience of caring directly for patients in a more minimal setting. Patients walked themselves directly to the OR, surgical instruments were scrubbed with steel brushes and sanitized in what Shepherd describes as a “small, microwave-sized autoclave.”

Hailey Shepherd, MD 
Meghan Kelly, MD 
SOfA surgical team
“Operating in El Salvador felt like being introduced to general surgery in its truest, simplest form,” Shepherd says. “We didn’t have any of the extra ‘stuff’ that accompanies surgery as we know it back home. For the first time, I learned what the essential ingredients of performing an operation were: there was no suction, no lap pads, no scrub tech, no entourage of staff bustling throughout the OR. Just you, an attending, an anesthesia provider, a stretcher to operate on, a sterile pack of instruments, and a bovie.”
Attending physicians served as scrub techs for the residents, guiding them as they performed various types of hernia repairs.
“We dissected hernia sacs bigger than grapefruits (one even contained a segment of colon!),” Shepherd recalls. “There were no pre-operative CT scans to reassure you beforehand—no knowing what you were about to get into as you cut through layers of tissue. It was a matter of trusting your hands, and your instincts. In one patient, a large umbilical bulge suspected to be a hernia turned out to be an intra-abdominal mass. Most striking of all was seeing the patients after surgery. Instead of grimacing and groaning in pain—as I would expect right after a large, open hernia repair—the patients would awaken in the OR and immediately turn to us, grabbing our hands and crying, repeatedly thanking us for helping them. There were no screens gluing our eyes or frivolous checkboxes to click through. We wrote the details of our operation with ink on a piece of paper and placed it in the patient’s chart beside them. It was a side of general surgery I hadn’t seen before—a moment to briefly detach from all of the things that surgery isn’t, and reconnect with everything that it is.”
Changing Lives Through Surgical Outreach
SOfA was founded by Peggy Frisella, BSN, who is the administrator of the Washington University Institute for Surgical Education (WISE), and Brent Matthews, MD, a past chief of the Section of Minimally Invasive Surgery, in 2008. The nonprofit’s mission is to provide surgical services to the underserved in the developing countries of North, Central and South America.
More than a decade since their first trip, SOfA continues this mission through multiple week-long trips each year. In early 2022, Frisella and team led a mission to the Dominican Republic, where a group of 15 volunteer health-care professionals performed 85 surgical procedures and evaluated over 130 patients.
During both 2022 missions, the most common type of procedure was hernia repair surgery. Hernias are common around the world, but in countries without widespread resources for surgical repair, they can become a major medical problem. When a person relies on physical labor to make a living, hernia pain can be debilitating. Many people in the countries SOfA visits suffer from untreated hernias for months or years, often while continuing to work to provide for their families.
“Our surgical missions are so rewarding for us as health-care professionals, but they also make a big difference,” says Frisella. “Somebody who is in chronic pain and can’t work is unable to support their family’s needs. These are lifechanging surgeries.”
In addition to providing essential surgical care, SOfA offers training for local surgeons and residents. This investment in the community ensures that, even after a mission’s conclusion, people in the area have continued access to the care they need.

A Lifelong Passion
Leading a surgical nonprofit requires commitment and collaboration: two skills Frisella possesses in abundance. She has built lasting connections in the countries SOfA visits, empowering the organization to create a greater impact in local communities. Drawing on her 40-plus years of nursing expertise, Frisella has also established a network of health-care professionals to provide care on SOfA trips.
For Frisella, extending access to world-class health care to those in the greatest need is a lifelong passion. When she was 21, Frisella spent a year running a clinic in rural Guatemala. When her children were in high school, Frisella took each of them individually on a service trip.
Over the years, she has continuously expanded her reach, from early mission trips to formalizing SOfA’s status as a nonprofit to donating medical supplies when travel was impossible at the height of the COVID-19 pandemic.
During her years of leadership at SOfA, Frisella—who is also Manager of Research Operations at the Washington University Institute for Minimally Invasive Surgery—has published studies based on the organization’s experience, including an article titled “Building a Sustainable Global Surgery Nonprofit Organization at an Academic Institution,” published in the Annals of Global Health.
SOfA’s impact continues to grow. This year, the organization is helping to build two operating rooms in a particularly underserved area of Belize, which will create spaces for safe and effective surgical treatment for years to come. In Texacuangos, El Salvador, where Shepherd and Kelly recently volunteered, SOfA has initiated a new laparoscopic gynecology program, improving access to women’s health resources in the local area.
Frisella notes that mission trips like the ones to El Salvador and the Dominican Republic are made possible by charitable donations to SOfA, as well as the teams of volunteer medical experts who provide much-needed care. SOfA volunteers include physicians from around the St. Louis area and across the country. When the team includes Washington University surgeons and residents, it is especially rewarding for Frisella, who has been with the School of Medicine for over 35 years.
“Each SOfA trip is a team effort,” Frisella says. “It is a huge undertaking that requires a lot of preparation and dedication from the team. Over the years, Washington University has felt like a home base for SOfA. Our trainees and faculty have a real commitment to providing the best care, and the people we serve on our mission trips benefit from that expertise. But these trips change our lives as well. When our residents see the impact they can have on the lives of others, that stays with you.”