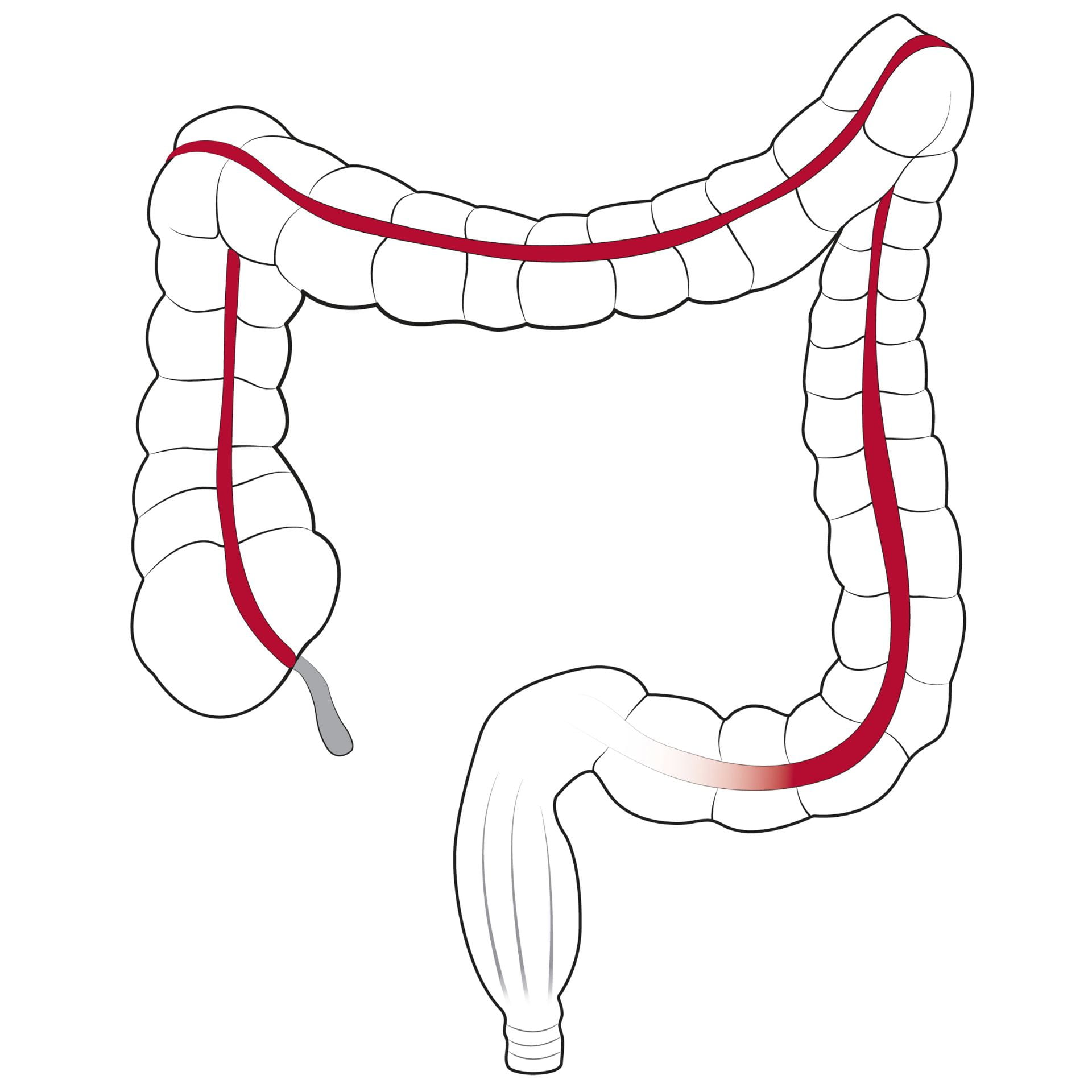
Building on a successful history, this section continues its role as a leader in research and treatment in all aspects of colorectal surgery. Surgeons provide collaborative and comprehensive care to patients with diseases of the colon, rectum and anus. Faculty are leaders in their field and have special expertise in laparoscopic colon surgery, offering this treatment for colon and rectal cancer, diverticulitis, ulcerative colitis, Crohn’s disease, colon polyps, rectal prolapse and chronic constipation. Surgeons apply basic science research to the clinical realm, offer several colorectal cancer clinical trials and train the next generation of surgical innovators through a one-year colorectal surgery fellowship.
Our Year In Numbers
2,719
operating room cases

16,263
visits

7
faculty

1,032
office procedures

27
clinical research studies
$237,616
research funding
Section of Colon and Rectal Surgery | 2022 Annual Report

Paradigm Shift in Treating Rectal Cancer
The Section of Colon and Rectal Surgery is one of the few centers in the country that is using short-course radiation therapy for rectal cancer. This treatment administers five days of short course radiotherapy, delivering the same biologic dose of radiation as the current standard of treatment in the United States in a shorter time. Systemic chemotherapy is then administered preoperatively. This complete treatment plan is now referred to as total neoadjuvant therapy.

Young-onset Colorectal Cancer Program Growth
Washington University colorectal surgeons, medical and radiation oncologists, and other specialists have partnered with Barnes-Jewish Hospital and Siteman Cancer Center to address the unique needs of young-onset colorectal cancer patients through a new program. The rising incidence of young-onset colorectal cancer led the American Cancer Society and the U.S. Preventative Services Task Force to revise its colorectal cancer screening guidelines in 2021 to start earlier at age 45 instead of 50 for individuals at average risk.
Highlights
CLINICAL

Sean Glasgow, MD, and Radhika Smith, MD, are part of the multidisciplinary team that provides diagnosis and treatment for benign anorectal and pelvic floor disorders at the Washington University Center for Colorectal and Pelvic Floor Disorders (COPE Center). Common ailments treated include urinary incontinence, bowel obstruction, hemorrhoids, perirectal abscesses, prolapse and pelvic pain. The center, located in Barnes-Jewish West County Hospital, was the first of its type in the Greater St. Louis area to bring together colorectal surgeons, urologists, urogynecologists and support staff to care for patients with these conditions and has recently seen significant clinical growth.
RESEARCH

Rectal surgery is often a major concern for patients because of its impact on quality of life and self-perception. The Section of Colon and Rectal Surgery participated in a multicenter three-year trial that found that the “watch-and-wait” method, in which physicians treat the patient with intensive radiation and chemotherapy to shrink or eliminate the tumor then closely monitor for recurrence, is a potentially rectum-preserving treatment approach for locally advanced rectal cancer. Steven Hunt, MD, is an author on a study’s findings, published in the Journal of Clinical Oncology. Washington University colorectal surgeons and residents are now developing a research project to study the decision-making process for patients considering organ preservation.
EDUCATION

Paul Wise, MD, who serves as the General Surgery Residency Program Director, was selected as an at-large member of the Association of Program Directors in Surgery’s (APDS) executive committee. The APDS is an organization that provides a forum for the exchange of information on subjects related to post-graduate surgical education. During this three-year appointment, Wise will assist in the management of the affairs of the Association and appointment of agents. The section also offers a one-year colorectal fellowship program, led by Program Director Matthew Silviera, MD, MS, and Associate Program Director Radhika Smith, MD. The program accepts three fellows each year.

Paradigm Shift in Treating Rectal Cancer
The Section of Colon and Rectal Surgery is one of the few centers in the country that is using short-course radiation therapy for rectal cancer.
This treatment administers five days of short course radiotherapy, delivering the same biologic dose of radiation as the current standard of treatment in the United States in a shorter time. Systemic chemotherapy is then administered preoperatively. This complete treatment plan is now referred to as total neoadjuvant therapy.
First chief and founder of the section Ira Kodner, MD, pioneered the use of short-course radiation in the 1980s, which then allowed surgeons to perform less radical surgical procedures for patients with rectal cancer. Section Chief Matthew Mutch, MD, and surgeon Steven Hunt, MD, are now leading the efforts at the School of Medicine to build on Kodner’s early success with the treatment.
“This legacy was built with Ira Kodner decades ago, and our institution has carried it forward with what we now term total neoadjuvant therapy,” says Mutch, who is the Solon and Bettie Gershman Professor of Surgery.
This strategy is used more frequently in European countries and has not been widely adopted by many centers in the United States. The section is making an impact on practice patterns within the region, however, as more radiation oncologists are utilizing short course therapy.
This year, William Chapman Jr., MD, MPHS, 2021-2022 Walter F. Ballinger II Administrative Chief Resident, led a multidisciplinary study that supports short-course radiation for rectal cancer.
This project was built on previous research performed at the School of Medicine, in which results of the RAPIDO (Rectal Cancer And Pre-operative Induction Therapy Followed by Dedicated Operation) clinical trial demonstrated the efficacy of this as a new standard for treating rectal cancer.
Researchers compared clinical performance and oncologic outcomes of two rectal cancer neoadjuvant treatment standards: short-course total neoadjuvant therapy versus standard chemoradiation. They found that the short-course total neoadjuvant therapy regimen correlated with improved tumor downstaging and similar progression-free survival of patients with rectal cancer when compared to other forms of chemoradiation.
The major benefit of total neoadjuvant therapy for patients are several. First, the radiation therapy consists of five days of treatment instead of five weeks of treatment. Second, by administering the chemotherapy before surgery, patients are more likely to begin and receive more doses of chemotherapy. Finally, this strategy appears to improve survival in patients with rectal cancer.
“What we have shown has been equivalent results to traditional long course radiation therapy with opportunity to improve the overall outcome for rectal cancer patients,” says Mutch. “This practice is becoming a major paradigm shift in how we are treating rectal cancer.”
The team presented their findings at the 2022 American Society of Colorectal Surgery annual meeting and is currently discussing joining a national research collaborative for further investigations to advance this treatment for rectal cancer.

Young-onset Colorectal Cancer Program Growth
Washington University colorectal surgeons, medical and radiation oncologists, and other specialists have partnered with Barnes-Jewish Hospital and Siteman Cancer Center to address the unique needs of young-onset colorectal cancer patients through a new program.
Colorectal cancer patients are considered young-onset if they are diagnosed before they turn 50 years old. Young-onset colorectal cancer is a growing problem. The rate of colorectal cancer in patients 49 and younger has increased by more than 50% in recent years. The rising incidence of young-onset colorectal cancer led the American Cancer Society and the U.S. Preventative Services Task Force to revise its colorectal cancer screening guidelines in 2021 to start earlier at age 45 instead of 50 for individuals at average risk.
“It is a population that has unique needs compared to your typical older cancer patient. They are working, they have young children,” says Chief of Colon and Rectal Surgery Matthew Mutch, MD. “You often envision a colon cancer patient as an older individual being accompanied by their adult children. Because of this significant shift toward earlier onset, a lot of the patients today are those kids.”
The Washington University young-onset cancer program offers a personalized treatment plan based on the patient’s needs. This multidisciplinary team-based approach allows physicians to work together to find the best solutions for patients, and often reduces the number of appointments a patient needs to schedule. The colon and rectal surgery team also includes skilled staff nurses, ostomy nurses, physicians’ assistants, and medical assistants. They work closely with leading experts in medical oncology, radiation oncology, pathology, and radiology to provide state of the art care with a focus on curing cancer the safest way possible.
This team is leading the region in the non-operative management of rectal cancer, minimizing the need for surgery unless necessary.
In addition to the team of experienced physicians, the young-onset colorectal cancer program includes access to the Living Well Center, which offers holistic care to patients including acupuncture, physical therapy, medical massage, nutritional counseling, fitness classes and more. Other services available in the young onset cancer center include social services, genetic counseling, reproductive and sexual health, financial services, and rehabilitation.
The program has seen significant success and growth, doubling the number of patients treated since its start in early 2022.
“The young-onset cancer program has taken off,” says Mutch. “We have much more formalized care paths for patients in this program and have developed multidisciplinary workflows with medical oncology and radiation oncology.”
The program also partners with researchers in the Division of Public Health Sciences, who are leading efforts to discover the genomic landscape of young-onset colorectal cancers and the underlying lifestyle factors that may drive the rising incidence.