
Washington University pediatric cardiothoracic surgeons treat children with congenital cardiac disorders. Washington University specialists treat a wide range of conditions, from atrial septal defects to complex single ventricle anomalies, neonatal surgery, surgery for congenital heart disease and tracheal reconstruction. The lung transplant program at St. Louis Children’s Hospital is among the most active of its kind in the world, attracting patients with cystic fibrosis and other lethal lung diseases from around the globe. The pediatric heart transplant program is considered a national leader in the specialty. The section also offers advanced training through an ACGME-accredited congenital cardiothoracic surgery fellowship.
Our Year In Numbers
1,027
operating room cases

1,420
visits

4
faculty

30
clinical research studies
$215,473
research funding
Section of Pediatric Cardiothoracic Surgery | 2022 Annual Report

A Beautiful New Heart: Audrey’s Story
This March, Audrey celebrated her first birthday at home with her family. Audrey’s mother, Molly Wallach, as an assistant nurse manager at the St. Louis Children’s and Washington University Heart Center, knew there was a chance Audrey would spend her first birthday in a hospital room.
A Hands-On Approach to Learning
After gaining valuable experience during an in-depth, hands-on training experience, Washington University pediatric cardiothoracic surgeons and fellows can utilize new tools to diagnose and plan treatment strategies for patients with rare and complex heart defects.
Highlights
CLINICAL

Washington University pediatric cardiothoracic surgeons provide the highest quality care to patients with congenital heart defects. To ensure the program’s continued excellence, the team engages in several rigorous practices to regularly review performance and outcomes. During monthly performance improvement rounds, the team reviews each patient’s hospital course from admission to discharge, comparing their findings to a national database and determining what lessons can be learned to continuously improve. This practice seeks to enhance dialogue across disciplines by recognizing both areas for improvement and the team’s successes. Surgeons from the section also follow up with patients and caregivers to examine long-term outcomes and evaluate the durability and effectiveness of treatments.
RESEARCH

Tetralogy of Fallot is a congenital heart defect that affects normal blood flow through the heart. Pirooz Eghtesady, MD, PhD, and his research team are developing a novel surgical technique using heart tissue to treat Tetralogy of Fallot. In 2022, the team presented a 14-year evolution of management of the pulmonary valve using living right atrial appendage tissue, concluding that this method of repair is a safe operation with excellent outcomes. A second study describes a technique for complete repair of Tetralogy of Fallot with other defects using right atrial appendage tissue. This technique provides advantages of right heart protection and the use of living tissue capable of growth with the patient.
EDUCATION
In 2020, the Section of Pediatric Cardiothoracic Surgery introduced an ACGME-accredited Congenital Cardiac Surgery Fellowship, one of only 11 congenital cardiac fellowships in the country. This program now accepts one distinguished fellow every other year. Training through this program provides opportunities for cardiothoracic surgeons to develop the expertise necessary for subspecialization in congenital cardiac surgery. Inaugural fellow Jacob Miller, MD, joined the Section of Pediatric Cardiothoracic Surgery at Washington University School of Medicine in St. Louis in 2021 as an instructor of surgery. The most recent fellow, Vinod Sebastian, MD, finished his pediatric cardiothoracic fellowship and now works as a pediatric cardiac surgeon with University of California, San Francisco.

A Beautiful New Heart: Audrey’s Story
This March, Audrey celebrated her first birthday at home with her family. Audrey’s mother, Molly Wallach, as an assistant nurse manager at the St. Louis Children’s and Washington University Heart Center, knew there was a chance Audrey would spend her first birthday in a hospital room.
Audrey was diagnosed with a congenital left ventricular aneurysm before she was born and dilated cardiomyopathy at three weeks old. This combination of rare heart conditions required multiple operations, including a heart transplant at only six months old. Thanks to an organ donor and the team of specialists at the Heart Center, Audrey is now a happy, healthy one-year-old girl.
Audrey’s Heart Center team included Pirooz Eghtesady, MD, PhD, Cardiothoracic Surgeon-in-Chief at St. Louis Children’s Hospital, as well as Washington University congenital cardiac surgeons Jacob Miller, MD, and Dilip Nath, MD.
“Dr. Eghtesady has such a calm confidence,” Wallach says. “I remember him coming up to me on the night of Audrey’s first surgery, putting his hand on my shoulder and saying, ‘I’m going to take care of your daughter.’ I was so scared, but then I felt this rush of relief. I knew that Dr. Eghtesady would go to the ends of the earth for Audrey.”
At three months old, Audrey underwent VAD placement. She spent just over three months awaiting a transplant in the hospital, supported by her VAD, her care team and the love of her family.
The Heart Center is a nationally recognized Mechanical Assist Device program. Placing a VAD in a left ventricular aneurysm is an exceptionally rare procedure, but Wallach knew her child was in good hands with Eghtesady, who is also chief of pediatric cardiothoracic surgery at Washington University.
“As a practitioner, it was anxiety provoking that I was caring for one of our own,” says Eghtesady. “At the same time, the trust and privilege the Wallach’s provided us by trusting Audrey’s care in our hands was a testament to the relationship as well as a precious vote of confidence in our team. I am grateful they would trust Audrey’s surgery to us and that we were able to provide her with a great outcome.”
After an unusual first year, Audrey is now back home with her family, vibrant and healthy. “We want Audrey to experience life,” Wallach says. “Drs. Eghtesady, Miller and Nath always remind me that, at the Heart Center, we choose transplant because we want kids to live. Now that Audrey has a beautiful new heart beating in her chest, we’re going to let her live a normal life.”
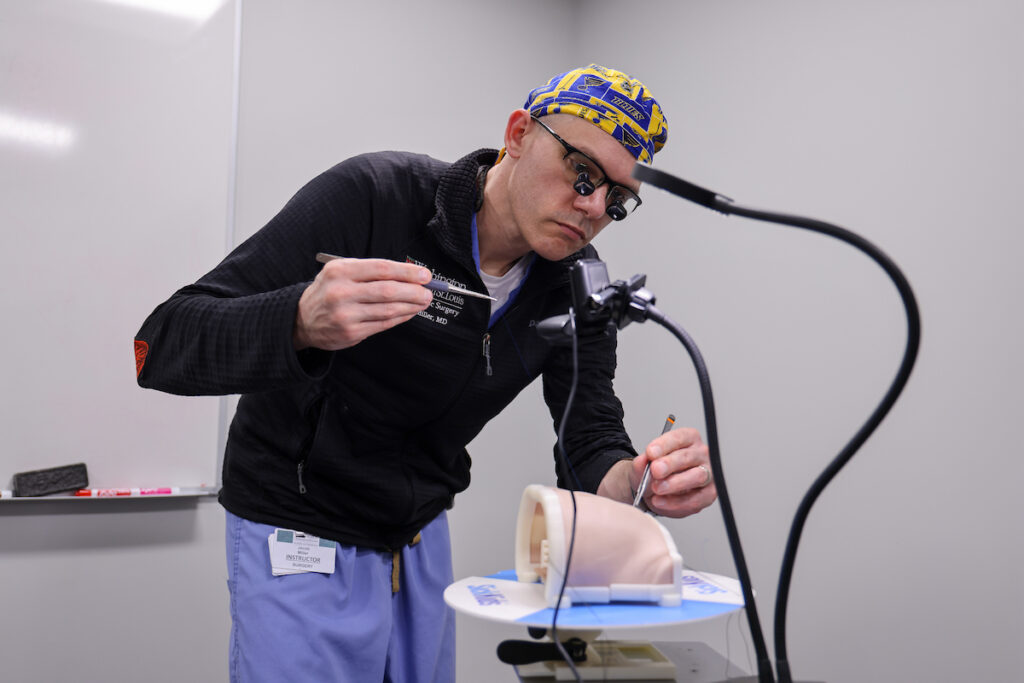
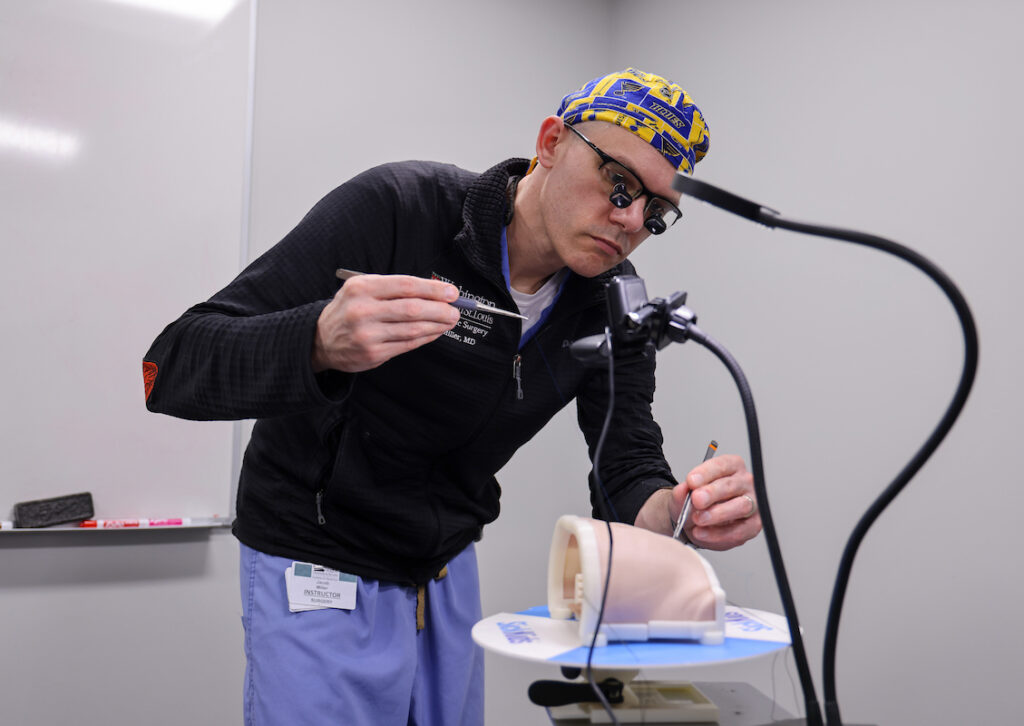
A Hands-On Approach
This year, pediatric cardiothoracic surgeons joined a specialized training program tailored around treating congenital heart defects. The HOST (Hands-On Surgical Training) program, led by cardiovascular surgeons from the Hospital for Sick Children in Toronto, Canada, guides surgeons from around the world through the repair of complex heart defects utilizing realistic simulation models. The team from Washington University were the only surgeons from the U.S. that participated in the session.
Though the Section of Pediatric Cardiothoracic Surgery currently utilizes 3D models in preoperative planning, trainee education and patient education at St. Louis Children’s Hospital, the HOST program gives the surgeons a new perspective in treating congenital heart conditions.
“We were astounded by the level of detail shown in the specially prepared silicone models used in this program,” says Pediatric Cardiothoracic Surgery Section Chief Pirooz Eghtesady, MD, PhD. “The models, designed in accordance with real defects captured by CT or MRI imaging, were 3D-printed, assembled and shipped to our team.”
Following an introductory preparatory course, trainees and faculty members practiced simulated procedures, such as extended end-to-end coarctation aorta repairs and Norwood procedures, on the complex models with guided instructions.
“In patients with complex disease, these models provide a great resource and allow for one to really visualize pathology. The models are the closest thing to mimic actual surgery that I’ve ever seen,” says Jacob Miller, MD, an instructor of pediatric cardiothoracic surgery. “They also act as a great reference to facilitate discussion with the faculty and discuss tips and tricks used to optimize the repair.”
“Since the session was conducted in a virtual environment with a webcam spotlighting the surgical area and model, surgeons received real-time feedback from the course proctors during their procedures and received a final review of their approaches and anatomic results,” says Eghtesady, cardiothoracic surgeon-in-chief at St. Louis Children’s Hospital. “We are happy to report the patients did well under the hands of our surgeons.”
Following the success of the initial training program, the division conducts ongoing simulation training monthly as part of its comprehensive surgical training curriculum.