Washington University vascular surgeons have been providing leading-edge quality patient care since the establishment of the service in 1983. This section offers open and endovascular treatment for patients with vascular disease and participates in clinical trials of stent graft devices to treat thoracic aneurysms using endovascular techniques. Faculty provide innovative clinical training in residency and fellowship programs accredited by the Accreditation Council for Graduate Medical Education. Members of the section lead basic science, translational research, clinical outcomes and novel device trials, and they support the education of the numerous general surgery residents in rotation on the service.
Our Year In Numbers
3,082
operating room cases

15,203
visits

12
faculty

188
office procedures

47
clinical research studies
$1,699,539
research funding
Section of Vascular Surgery | 2022 Annual Report

The Washington University CardioVascular Research Innovation in Surgery and Engineering (CVISE) Center is a program combining the training, knowledge and skill sets of post-doctoral surgeon-scientists and pre-doctoral engineering students to foster the growth of cardiovascular research innovators. The program provides strong foundations in cardiovascular pathophysiology, basic and translational research, applicable engineering principles, entrepreneurship, and an understanding of responsible partnerships with industry and pathways for commercialization.
John Felder, MD, John Kirby, MD, Grant Bochicchio, MD and Justin Sacks, MD, MBA.
Collaborative Limb Preservation
Diabetes and peripheral arterial disease are limb threatening conditions that contribute significantly to rising amputation rates in the United States. For many individuals, limb loss is associated with depression, increased lifetime health care costs and increased risk of further amputations. Washington University vascular surgeons, in partnership with a multidisciplinary team of specialists, are helping a growing number of patients avoid amputations through a comprehensive limb preservation program.
Highlights
CLINICAL

Washington University vascular surgeons are pioneering aortic surgical techniques through clinical trials of novel devices. Some devices recently studied at Washington University are now approved for patient care, while other devices being tested today have had significant early successes in clinical trials. “These devices have the potential to completely change the management of patients with complex thoracoabdominal disease,” says Section Chief of Vascular Surgery Luis Sanchez, MD. Sanchez and cardiac surgeon, Puja Kachroo, MD, are collaborating to develop a multidisciplinary aortic surgery program, consolidating the expertise of these surgical specialties to streamline long-term patient care.
RESEARCH

Katherine Holzem, MD, PhD, joins the division with a focus on basic science and translational research in peripheral vascular disease. Holzem has extensive background as both a surgeon and investigator. She earned her medical degree and doctorate from the School of Medicine in 2015 and completed her vascular surgery residency at Washington University this year. “Dr. Holzem will bring together research and clinical expertise to advance patient care and embody the mission of the medical school,” says Luis Sanchez, MD, who is the Gregorio A. Sicard Distinguished Professor of Vascular Surgery. “Her passion for cardiovascular disease research will enable us to bring new discoveries from bench to bedside for a growing patient population.”
EDUCATION

The vascular surgery fellowship program has grown to train two fellows every year. With a high clinical volume of vascular surgery at Washington University allowing for more hands-on experience, this expansion will increase the mentorship of more trainees in vascular surgery. Faculty including Luis Sanchez, MD, and J. Westley Ohman, MD, are committed to training and mentorship, which benefits all surgeons in the section. “Our fellows bring added training opportunities for junior residents,” says Sanchez. Fellows, including Gayan De Silva, MD, who received the Gregario A. Sicard Fellow Teaching Award this year and the Eugene M. Bricker Teaching Award last year, also contribute to the mentorship of residents across the department.

A Foundation of Innovation
The Washington University CardioVascular Research Innovation in Surgery and Engineering (CVISE) Center is a program combining the training, knowledge and skill sets of post-doctoral surgeon-scientists and pre-doctoral engineering students to foster the growth of cardiovascular research innovators. The program provides strong foundations in cardiovascular pathophysiology, basic and translational research, applicable engineering principles, entrepreneurship, and an understanding of responsible partnerships with industry and pathways for commercialization.
The program, established in 2022, offers trainees foundational experiences to encourage collaboration and inspire independence as investigators. It serves as a pipeline for cardiovascular research innovators to make lasting impacts on the future of surgical technology and practice. Trainees are provided access to mentorship across a wide span of surgical specialties in addition to career advisors and an entrepreneurial and commercialization committee. These opportunities offer trainees not only a space to innovate, but also a team committed to helping them navigate the process of creating and implementing their innovations in the field.
CVISE is home to a multidisciplinary team of expert faculty serving as collaborators and mentors. Program Director Mohamed Zayed, MD, PhD, is an associate professor of surgery and radiology and a mentor within the program. His research laboratory studies a wide range of vascular pathologies, including peripheral arterial atheroprogression, arterial aneurysmal disease and deep venous thrombosis. His team combines bioengineering principles to discover translational research solutions to complex cardiovascular problems. Associate program directors include Christian Zemlin, PhD, who leads the Cardiac Surgery Research Laboratory, and Plastic and Reconstructive Surgery Residency Program Director Alison Snyder-Warwick, MD.
“What’s exciting about the CVISE training program moves beyond traditional examples of individual collaboration and innovation. Instead, this program aims to build on existing infrastructure, and a track-record of successful collaboration between surgery and engineering to develop new thought leaders in the field of cardiovascular surgery,” says Zayed. “Side-by-side, surgeons and engineers, primary mentors and trainees, will collaborate and synergize on projects that will accelerate the advancement of their research topics, help them develop new important skillsets, build a community of innovators and problem-solvers, and support trainee future professional research careers in academia and/or industry.”
Inaugural CVISE fellow Sophia Roberts, MD, a PGY-2 general surgery resident, is currently evaluating a suite of devices being repurposed for cell-based and drug-based therapy to cure a wide-range of cardiovascular diseases. Under the mentorship of Zayed and Chief of Cardiothoracic Surgery Ralph Daminao, MD, Roberts will further develop and hone her research interests in cardiovascular surgery, with special interests in transplantation, mechanical circulatory support and aortic surgery.
Collaborative Limb Preservation
Diabetes and peripheral arterial disease are limbthreatening conditions that contribute significantly to rising amputation rates in the United States. For many individuals, limb loss is associated with depression, increased lifetime health care costs and increased risk of further amputations.
Washington University vascular surgeons, in partnership with a multidisciplinary team of specialists, are helping a growing number of patients avoid amputations through a comprehensive limb preservation program. A major sign of this program’s success is the addition of faculty members focused on the treatment and research of limb-threatening conditions.
Genevieve Hayek, MD, whose clinical focus is on limb preservation, joins the section as an assistant professor. Hayek recently completed her vascular and endovascular fellowship at Washington University School of Medicine. She earned her medical degree from the University of Queensland School of Medicine in Queensland, Australia in 2014 and completed her general surgery residency at Ochsner Clinic Foundation at Ochsner Medical Center in New Orleans, Louisiana in 2020.
“The great thing about a limb preservation program like the one at Washington University is that we work in close collaboration with podiatry, plastic surgery, acute care surgery and wound care to provide our patients with the best possible chance of preserving their limbs,” says Hayek. “We are able to utilize the talents and resources of many different groups to fully and creatively tackle these often difficult and complex problems. As a surgeon, it is immensely rewarding to see our patients benefit from our efforts.”
This clinical mission is further supported by the research programs of Mohamed Zayed, MD, PhD, whose laboratory aims to understand what makes certain patient populations more at risk of developing major artery blockages in the extremities, and Katherine Holzem, MD, PhD, a surgeon-scientist with a research focus on limb-threatening conditions.
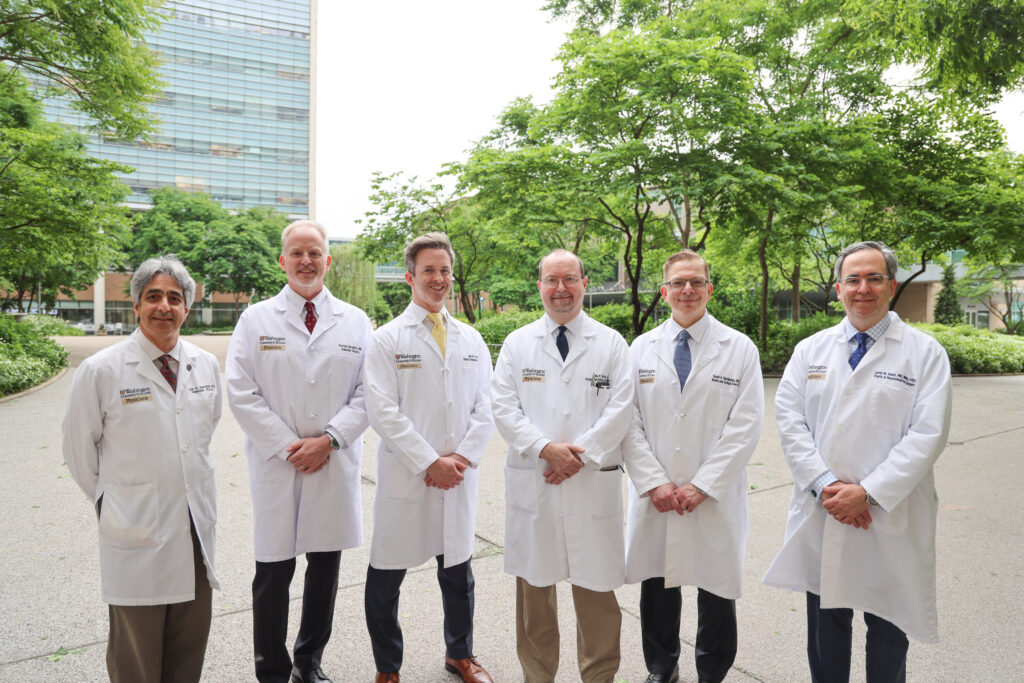
The addition of these skilled physicians will support the expertise and reach of the limb preservation program as it provides testing, diagnosis, treatment and recovery to its patients with conditions like diabetic foot ulcers, chronic limb-threatening ischemia, peripheral arterial disease and venous disorders. The program is further strengthened by the input of multidisciplinary experts and physicians. The limb preservation program combines expertise in podiatry, acute and critical care surgery, plastic and reconstructive surgery, orthopedics and vascular surgery to meet the needs of patients. Patrick Geraghty, MD, leads the program as co-director alongside John Felder, MD, from plastic and reconstructive surgery and John Kirby, MD, from acute and critical care surgery.
Physicians from all of these disciplines are nationally and internationally recognized for their involvement in innovative clinical trials to improve treatment options, and their contribution to the limb preservation program helps set a new standard of excellence through patient care, research and education initiatives.