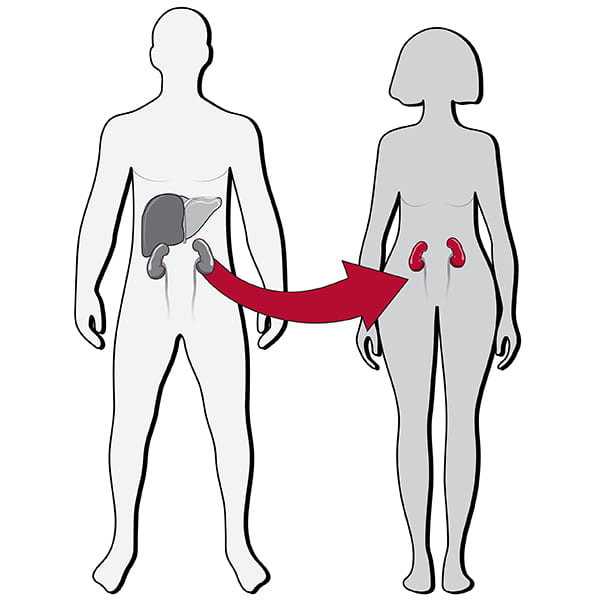
This section has a long, successful history of pioneering new clinical techniques and continues to lead advancements in the field. In liver transplantation, the program offers living-related and living-unrelated donor, reduced-size liver, split liver and dual-organ transplantation. Faculty offer both laparoscopic and “mininephrectomy” kidney donor procedures as well as robotic kidney transplantation. Transplant surgeons are at the forefront of research and development in islet cell transplantation and have the largest pancreas transplant program in the region. Along with their clinical expertise, faculty are leaders in the field of transplantation research and train fellows in a nationally recognized, two-year certified program.
Our Year In Numbers
1,322
operating room cases

9,627
visits

9
faculty

57
clinical research studies
$1,263,138
research funding
Section of Transplant Surgery | 2022 Annual Report

Washington University has a long history of making great strides in the field of transplant surgery. In 1963, the first kidney transplant in the Midwest was performed by Dr. William Newton at BarnesJewish Hospital. Today, this groundbreaking legacy is carried by the dedicated surgeons and investigators in the transplant program. In the last two decades, the total number of organ donors in the St. Louis region has increased by more than 140%. The partnership founded between Washington University School of Medicine, Barnes-Jewish Hospital and Mid-America Transplant has dramatically increased the volume of transplants. Together, they are addressing some of the most critical problems in transplantation today.

Full-spectrum Robotic Kidney Transplant
Over the last five years, Washington University surgeons have built one of the world’s largest programs for robotic kidney transplantation and HPB-GI surgery. These fields have historically been associated with large incisions. Technological advances, institutional investments and world-class surgical skill have empowered Washington University surgeons to offer patients the latest minimally invasive options for these major operations. The program is led by Adeel Khan, MD, MPH, who is director of robotic transplantation in the Department of Surgery.
Highlights
CLINICAL

Historically, liver cancer has been considered a contraindication for transplantation. A new national effort focuses on developing transplant strategies for liver cancer when other treatments are not feasible. The Washington University transplant program is one of the leading sites in this effort. The department has published data on ten-year outcomes of liver transplant and downstaging for hepatocellular carcinoma, and other research in cholangiocarcinoma, intrahepatic cholangiocarcinoma and metastatic colorectal cancer have led to successful treatment in otherwise untreatable cancer patients. Transplant faculty including William Chapman, MD, and Maria B. Majella Doyle, MD, MBA work to “downgrade” the stage of liver cancer before transplant and implement neoadjuvant treatment strategies in different cancers to increase patient survival.
RESEARCH
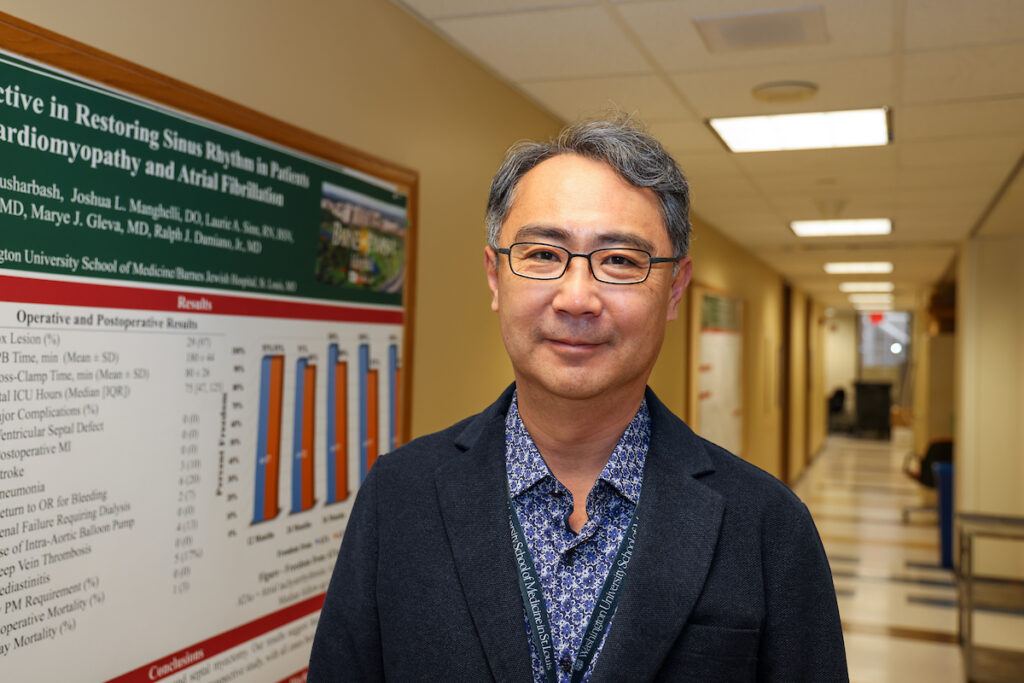
Jae-Sung Kim, PhD, is conducting pioneering research on the causes of and mitigation strategies for ischemic reperfusion injury. His recent publications describe factors that worsen injuries in the liver during ischemia/reperfusion, as some livers cannot tolerate ischemia reperfusion injury and are thus not eligible for transplant. Kim has many years of research experience in this space using cell and animal models, and his major research emphasis is to understand the molecular and cellular mechanisms underlying liver injury. Kim’s research ultimately seeks to develop novel therapeutic strategies to improve liver function after ischemia/reperfusion so more livers will be eligible for transplant.
EDUCATION
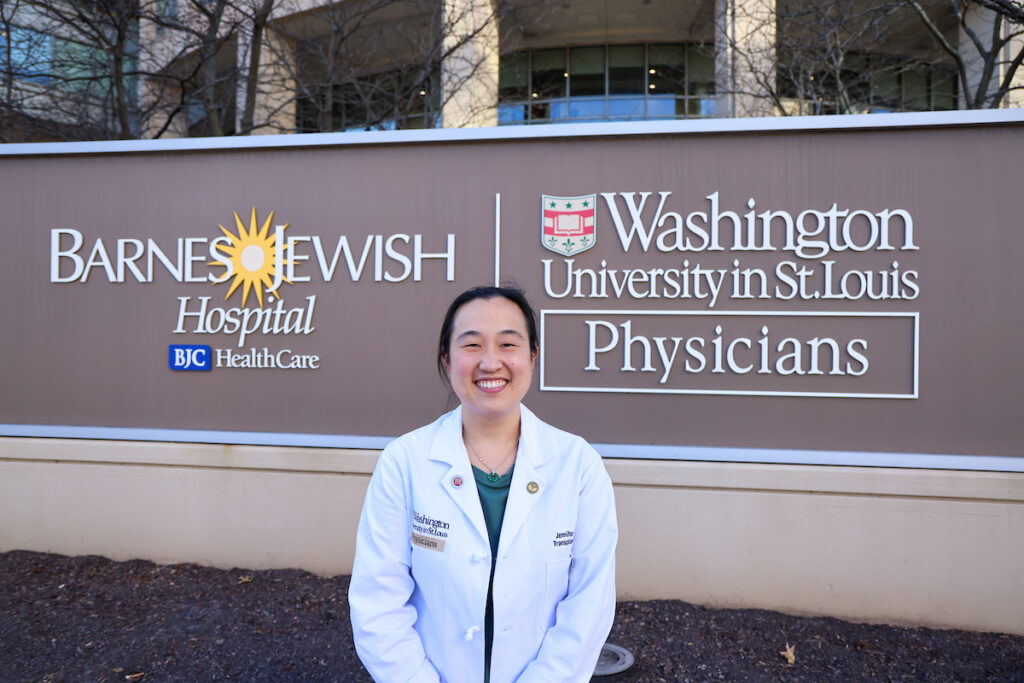
Jennifer Yu, MD, MPHS, joins the section as an assistant professor of surgery associate program director for the general surgery residency. Yu has earned her undergraduate, medical and master of population health sciences degrees at Washington University, where she also completed the T32 Surgical Oncology Clinical Research Fellowship, general surgery residency and an abdominal transplant fellowship under Maria B. Majella Doyle, MD, and Jason Wellen, MD, MBA. Among many other awards, Yu received the 2020-2021 Gregario A. Sicard Teaching Fellow Award from the general surgery residents as well as the 2020- 2021 Clinical Educator of the Year Award from students at the School of Medicine.

Partners in Progress
Washington University has a long history of making great strides in the field of transplant surgery. In 1963, the first kidney transplant in the Midwest was performed by Dr. William Newton at BarnesJewish Hospital. Today, this groundbreaking legacy is carried by the dedicated surgeons and investigators in the transplant program. In the last two decades, the total number of organ donors in the St. Louis region has increased by more than 140%. The partnership founded between Washington University School of Medicine, Barnes-Jewish Hospital and Mid-America Transplant has dramatically increased the volume of transplants. Together, they are addressing some of the most critical problems in transplantation today.
Leaders in the department, including Professor of Surgery Jae-Sung Kim, PhD, and Chief of Transplant Surgery William Chapman, MD, are investigating and developing solutions for the unique problems facing transplant surgery. Kim’s research investigates the roles of mitochondria and autophagy in ischemic liver injury and develops therapeutic strategies to reduce ischemia reperfusion injury in fatty livers. Chapman, the Eugene M. Bricker Professor of Surgery, leads the groundbreaking RESTORE trial.
The trial, which utilizes normothermic machine perfusion (NMP) technology on donated livers destined to be discarded by other facilities due to lack of confidence in organ quality, recently completed its second phase. These perfused livers have achieved successful results similar to those in cases with typically accepted donor livers. “We have transplanted 15 patients on this protocol in the last year and a half,” says Chapman. “Our goal is to get more people transplanted safely and effectively.”
Director of liver transplant at both Barnes-Jewish Hospital and St. Louis Children’s Hospital, Maria B. Majella Doyle, MD, MBA, exemplifies the leadership and clinical excellence of the department. Doyle, Mid-America Transplant/Department of Surgery Distinguished Endowed Chair in Abdominal Transplantation, is a renowned surgeon; the transplants and other procedures she performs transform the lives of some of the sickest patients, putting them on the path to recovery and giving them the chance to live a normal healthy life. Doyle’s leadership and contributions to the field were recognized at a chair installation ceremony hosted by the Foundation for Barnes-Jewish Hospital earlier this year, where she received the Mid-America Transplant/Department of Surgery Distinguished Endowed Chair in Abdominal Transplantation.
The leadership of dedicated faculty, alongside clinical partnerships, advanced surgical training and groundbreaking research in the transplant program, has advanced the field as a whole and delivered the highest quality of care to an ever-expanding volume of transplant patients.

Full-spectrum Robotic Kidney Transplant
Over the last five years, Washington University surgeons have built one of the world’s largest programs for robotic kidney transplantation and HPB-GI surgery. These fields have historically been associated with large incisions. Technological advances, institutional investments and world-class surgical skill have empowered Washington University surgeons to offer patients the latest minimally invasive options for these major operations.
The robotic kidney and HPB-GI program encompasses the full spectrum of these fields, from donor nephrectomy and kidney transplant to liver, pancreas, bile duct and stomach cancer, as well as nonmalignant conditions such as acute and chronic pancreatitis, liver cysts, bile duct injuries, gallbladder problems and pancreatic cysts. The program is led by Adeel Khan, MD, MPH, who is director of robotic transplantation in the Department of Surgery.
“We are one of very few centers to provide comprehensive experience in both HPB and transplant surgery,” says Khan. Many programs perform some robotic surgery—such as donor nephrectomies or a limited range of HPB-GI procedures—cover the breadth of both specialties.
Establishing a robotic program takes time and a team with dedication and expertise. The team includes Meranda Scherer, MSN, CRNFA, transplant surgery resource nurse and robotic first assist, as well as transplant surgeons Jason Wellen, MD, MBA, and Maria B. Majella Doyle, MD, MBA. A robotic program also requires access ORs equipped with surgical robots. Infrastructure investments of institutional leadership, including Jackie Martin Jr., MD, MBA, vice president of perioperative services at Barnes-Jewish Hospital, were critical.
The program performs approximately 150 robotic cases per year. The team also trains abdominal organ transplant fellows. Graduates have joined teams at major hospitals and medical schools across the country, where they will grow or establish robotic programs to serve more patients nationwide. Jennifer Yu, MD, who joined the faculty in August 2022, completed her transplant fellowship at Washington University.
New technology and high clinical volume are about providing the best experience and outcomes to patients. Washington University surgeons aim to expand that quality of care to as many patients as possible. Washington University surgeons have led training sessions for transplant programs from across the country.
About 20 programs have come to Washington University for guidance in growing their own robotic practice. These teams are drawn to the program’s high clinical volume and surgical success, as well as the fact that Washington University Medical Center is the first center in the country to be named an official Intuitive Surgical Training Center.
“Our vision is to continue the growth of our robotic transplant program and be the national leaders in this field,” says Khan.