Washington University cardiac surgeons, as part of the highest-ranked heart program in Missouri by U.S. News & World Report, have a long history of performing a spectrum of adult cardiac surgeries and are widely recognized as surgical leaders. Working with cardiologists, vascular surgeons, anesthesiologists, intensivists, and a highly qualified, experienced nursing staff, cardiac surgeons offer the latest advances in technology and innovative therapies. They also employ practices supported by scientific evidence as they strive to achieve the best possible outcomes for their patients.
2,895
Operating room cases
5,996
Visits
$2,350,974
Research funding
10
Faculty
82
Clinical research studies
Section of Cardiac Surgery | 2021 Annual Report

Washington University cardiac surgeons continue to advance the most innovative techniques in transcatheter therapies for valvular diseases. Transcatheter therapies are minimally invasive procedures with shorter recovery times than open surgery and rewarding patient outcomes. Over the last decade, industry developers have put forward numerous devices for clinical study.
Christian Zemlin, PhD, MSc, has been named director of the Cardiac Surgical Research Laboratory in the Division of Cardiothoracic Surgery at Washington University School of
Medicine in St. Louis. Zemlin, whose work focuses on the mechanisms and treatment of arrhythmias, was recruited from Old Dominion University in Norfolk, VA, where he served as graduate program director of the Biomedical Engineering Program.
Section of Cardiac Surgery Highlights | 2021 Annual Report

Clinical
Hypertrophic obstructive cardiomyopathy (HOCM) is a genetic disorder that causes thickening of the heart muscles and obstructs blood flow from the heart. Septal myectomy surgery, the treatment of choice for HOCM, provides long-term symptom relief and survival. Cardiothoracic Surgery Division Chief Ralph Damiano, Jr., MD, has performed minimally invasive HOCM procedures for nearly two decades. The minimally invasive procedure has resulted in less blood loss, shorter ICU length of stay and better postoperative pulmonary function for patients. Cardiac surgeon Kunal Kotkar, MD, joins Damiano in performing septal myectomies at the Washington University Hypertrophic Cardiomyopathy Center, the only National Hypertrophic Cardiomyopathy Association Center of Excellence in the region.

Research
The 2021 St. Louis Shock Symposium, led by Director of the Extracorporeal Life Support Program at Barnes-Jewish Hospital Muhammad Faraz Masood, MD, focused on critical conditions such as cardiogenic shock, COVID-19 related acute respiratory distress syndrome and pulmonary embolism. Washington University surgeons, including Masood, Kunal Kotkar, MD, and Varun Puri, MD, who have played a vital role in treating the most critically ill patients during the COVID-19 pandemic, presented research and clinical experience with these conditions. Health care professionals from across the region attended the conference to learn from leading experts and understand the optimal treatments for patients with cardiogenic shock and severe respiratory distress.

Education
While cardiac surgeons nationwide are trending towards private practice following their training, the Washington University cardiothoracic training programs continue to produce cardiac surgeons with an interest in academic surgery. Cardiothoracic Surgery Residency Program Director Varun Puri, MD, MSCI, provides advanced training while also maintaining an emphasis on wellness in the training program. “Because of the environment they have been part of at Washington University, our cardiothoracic trainees do not consider their training to be an end point, but rather the beginning to their academic career educating future generations of surgeons,” says Cardiac Surgery Section Chief Marc Moon, MD.

Leading the Charge in Transcatheter Therapies
Washington University cardiac surgeons continue to advance the most innovative techniques in transcatheter therapies for valvular diseases. Transcatheter therapies are minimally invasive procedures with shorter recovery times than open surgery and rewarding patient outcomes. Over the last decade, industry developers have put forward numerous devices for clinical study.
“One of the unique things about Washington University is that our high clinical volume and surgical expertise allow us to participate in almost all studies of new devices,” says Cardiac Surgery Section Chief Marc Moon, MD, the John M. Shoenberg Professor of Surgery. “Some of these devices will prove to be excellent replacements for more invasive techniques. Some may create opportunities for patients who presently have few therapeutic options.”
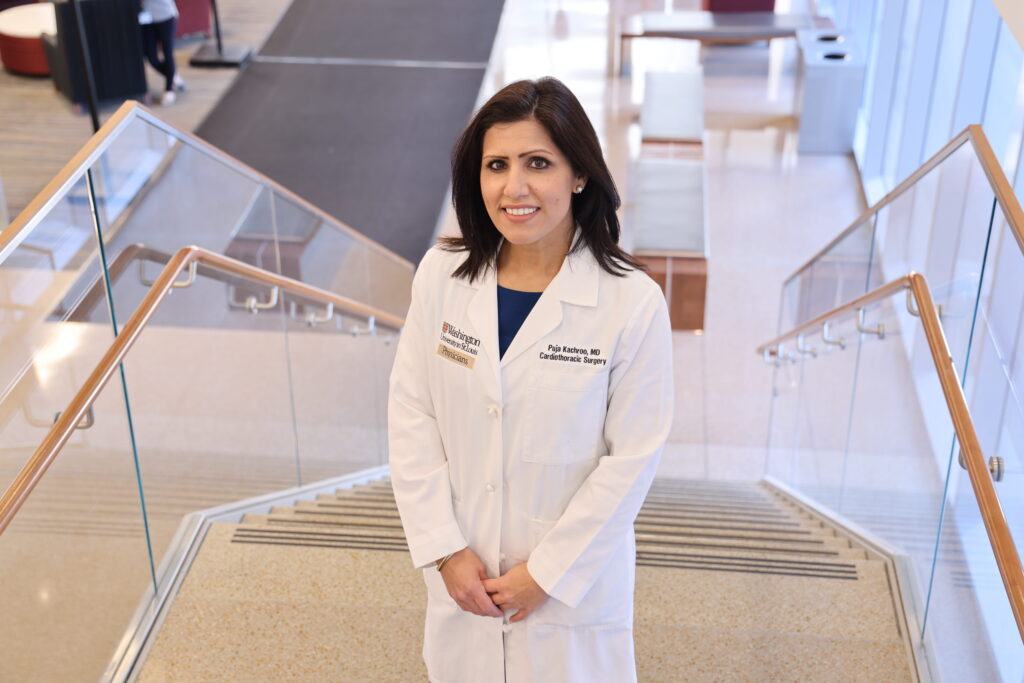
Leading the charge in these investigations of transcatheter therapies is cardiac surgeon Puja Kachroo, MD. This year, Kachroo and the team at the Washington University and Barnes-Jewish Heart & Vascular Center performed one of the first transcatheter interventions for tricuspid valve disease.
“Our goal is to evaluate and treat patients with valvular heart disease expeditiously, in a multidisciplinary fashion, offering state of the art diagnostic and novel therapeutic surgical or catheter-based interventions, in order to provide exceptional care,” says Kachroo.
Transcatheter valve therapies originated with TAVR (transcatheter aortic valve replacement). TAVR is a treatment option for patients with aortic stenosis, one of the most common, insidious valve diseases in the United States. Many patients with aortic stenosis are considered too high-risk for invasive surgery because of their age, heart function or other comorbidities. TAVR provides a minimally invasive option for valve replacement. Led by Spencer Melby, MD, Washington University cardiac surgeons were among the first in the country to participate in TAVR clinical trials, and continue to innovate with the procedure today.
Christian Hospital in North St. Louis provides leading-edge heart procedures in a hybrid room equipped with advanced imaging technology and surgical capabilities. Cardiothoracic surgeon Shuddhadeb Ray, MD, MPHS, recently performed one of the first planned TAVR in TAVR procedures in the St. Louis area. For a TAVR patient whose original replacement valve has deteriorated over time, TAVR in TAVR is an option that utilizes additional prostheses for a second valve replacement. This procedure, for a patient with renal failure, was the first at Christian Hospital to use the carotid artery as an alternative access site for TAVR.
As the section continues to innovate in transcatheter therapies, patient care is at the forefront for Washington University cardiac surgeons. Through advanced multidisciplinary care, the Cardiac Surgery Section expands therapeutic options for patients with even the most challenging valvular diseases.
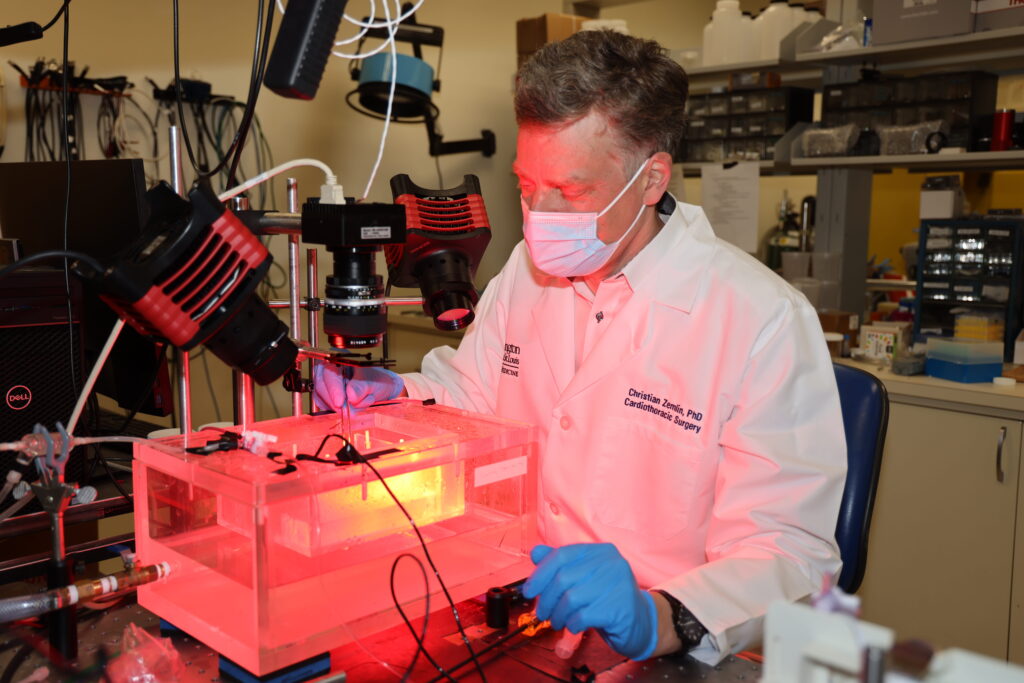
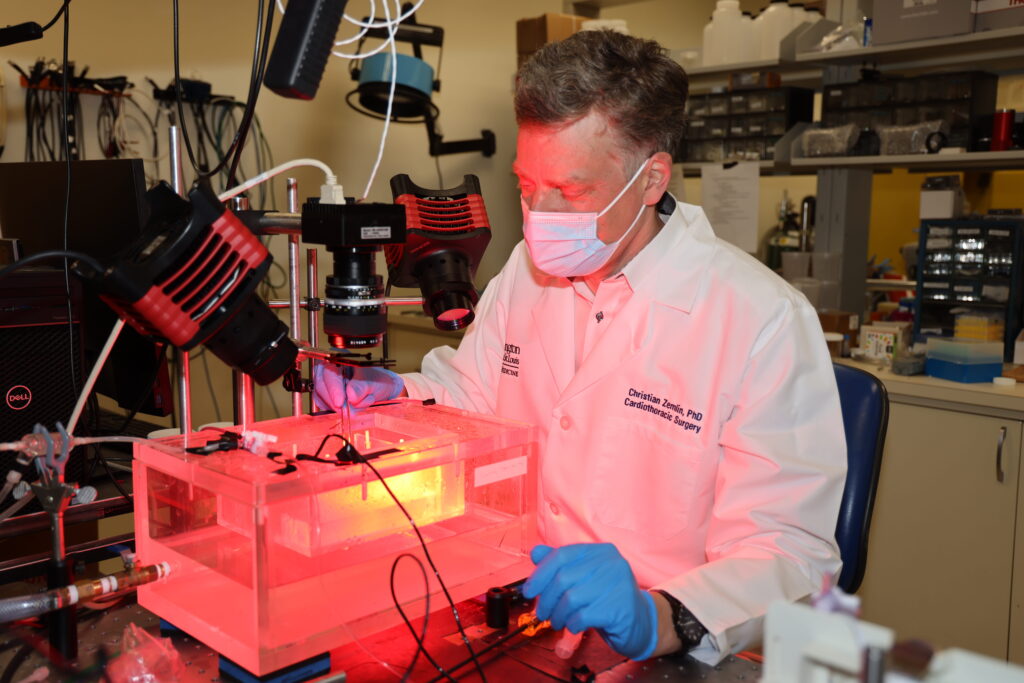
Shaping the Future of Cardiac Research
Christian Zemlin, PhD, MSc, has been named director of the Cardiac Surgical Research Laboratory in the Division of Cardiothoracic Surgery at Washington University School of Medicine in St. Louis. Zemlin, whose work focuses on the mechanisms and treatment of arrhythmias, was recruited from Old Dominion University in Norfolk, VA, where he served as graduate program director of the Biomedical Engineering Program.
“Christian will not only continue the exceptional work historically produced by our laboratory, but he will also put his own unique stamp on future productivity with his expertise in cardiac electrophysiology and biomedical engineering,” says Chief of Cardiothoracic Surgery Ralph Damiano, Jr., MD, the Evarts Graham Professor of Surgery.
In 2020, Richard Schuessler, PhD, retired after leading the research program for 20 years. A world-renowned scientist, Schuessler collaborated with a team of Washington University investigators and cardiac surgeons to rigorously evaluate ablation devices. Together, Schuessler and Damiano developed clinical innovations in the treatment of atrial fibrillation.
The mission of the Cardiac Surgical Research Laboratory is to solve the clinical problems that face cardiac surgeons. Among the many accomplishments of the continuously NIH-funded laboratory is the development of the Cox-Maze IV procedure—the first cure for atrial fibrillation. The laboratory also trains future scientists from around the world who will lead the field of cardiac surgery for generations to come.
Zemlin will continue this tradition of academic excellence by offering a formal training program for biomedical engineering students from the McKelvey School of Engineering.
“I am excited to continue the lab’s groundbreaking work on the surgical treatment of arrhythmias and to build new collaborations with WashU’s outstanding groups in biomedical engineering and cardiovascular research,” says Zemlin.
Zemlin earned a master’s degree in physics from the Technical University of Berlin in 1998 and a doctorate in theoretical physics from Humboldt University in Berlin in 2002. He completed his postdoctoral research in cardiac electrophysiology at SUNY Upstate Medical University in Syracuse. His research uses voltage-sensitive fluorescent probes to experimentally study cardiac activity, and computer modeling to understand how arrhythmias are initiated and maintained. Zemlin developed a new ablation modality for cardiac tissue based on ultrashort electric pulses that cause irreversible electroporation. His research has been funded by the American Heart Association, the NIH, intramural funding and industry.