
This section is dedicated to offering open and endovascular treatment for patients with vascular diseases. Surgeons also participate in clinical trials of stent graft devices to treat thoracic aneurysms using endovascular techniques. Faculty provide clinical training in residency and fellowship programs accredited by the Accreditation Council for Graduate Medical Education. Numerous general surgery residents also rotate on the service. Members of the section lead research in basic science, translational research, clinical outcomes and novel device trials.
2,770
Operating room cases
17,161
Visits
10
Faculty
194
Office procedures
42
Clinical research studies
$1,116,748
Research funding
Section of Vascular Surgery | 2021 Annual Report
The Vascular Surgery Residency Program at Washington University School of Medicine in St. Louis regularly attracts close to 100 applicants for a single position. Trainees benefit from high clinical volume, breadth of research experience and strong mentorship opportunities at an academic medical center committed to advancing health equity in St. Louis.

The Washington University and Barnes-Jewish Heart & Vascular Center offers advanced care for pulmonary embolisms at one of the best hospitals for cardiology, heart surgery and pulmonology, according to U.S. News & World Report. Washington University vascular surgeons are improving care pathways and treatment options for patients with pulmonary embolism and deep vein thrombosis through multidisciplinary collaboration and clinical research.
Section of Vascular Surgery Highlights | 2021 Annual Report

Clinical
The multidisciplinary Washington University Limb Preservation Program continues to save the limbs of patients at high risk for amputation. Program co-director Patrick Geraghty, MD, and vascular surgeons Westley Ohman, MD, and Vipul Khetarpaul, MD, see patients with peripheral arterial disease, chronic limb-threatening ischemia and other vascular diseases across the region. At Christian Hospital, Khetarpaul provides essential continuity of care for limb preservation patients. “A long-term care plan in a multidisciplinary fashion is really key in addressing the needs of this patient population to sustain the benefits they have received from an intervention, such as good function and circulation,” says Khetarpaul.

Research
Vascular Surgery Section Chief Luis Sanchez, MD, is a national leader in clinical research for the management of aortic arch disease and thoracoabdominal aneurysms. Clinical studies of recently developed devices have shown promising results for the endovascular treatment of patients with these complex conditions, who previously had few or no endovascular options. “If these devices prove successful, it is going to be a gamechanger in the management of thoracoabdominal aneurysms and aortic arch disease,” says Sanchez. “Because of our high clinical volume and surgical expertise, Washington University is a leading center in numerous promising studies.”

Education
Trainees in the Vascular Surgery Fellowship and Integrated Residency programs at Washington University School of Medicine in St. Louis remain engaged in research and educational activities while developing diagnostic and surgical skills at Barnes-Jewish Hospital. This year, residents presented research on endovascular and open repair of complex aortic disease at the Critical Issues America annual meeting. First year fellow Gayan De Silva, MD, who completed residency training at the School of Medicine this year, received the Eugene M. Bricker Teaching Award, an honor given to Chief Residents who demonstrate skills and passion for teaching.

A Vital Mission
The Vascular Surgery Residency Program at Washington University School of Medicine in St. Louis regularly attracts close to 100 applicants for a single position. Trainees benefit from high clinical volume, breadth of research experience and strong mentorship opportunities at an academic medical center committed to advancing health equity in St. Louis.
In 2021, the program accepted two residents: Margaret Nalugo, MD, and Shirli Tay, MD. Both Nalugo and Tay join the training program with significant vascular research experience. With the guidance of Vascular Surgery Residency Program Director Westley Ohman, MD, and the mentorship of vascular surgeon-scientist Mohamed Zayed, MD, PhD, these incoming residents have begun vascular surgery training with an impressive series publications, presentations and awards.
Nalugo received a 2021 Vascular Research Initiatives Conference (VRIC) Trainee Award for her research abstract titled “Towards A Cure For Diabetes: Pancreatic Tissue Encapsulation and Implantation In A Novel Arteriovenous Graft.” Mentored by Zayed, who is a Wiley Scholar Award recipient, Nalugo has completed additional training through the Training Opportunities in Translational Imaging Education and Research T32 training program at the Washington University Mallinckrodt Institute of Radiology.
Tay partnered with researchers from the Zayed laboratory to publish research on a blood marker that can accurately detect a severe type of peripheral artery disease. Led by Zayed, senior author and Director of the Vascular Surgery BioBank, the study was published in Scientific Reports. Tay received the 2020 Early Career Investigator Award from the American Heart Association and presented research at the VRIC in 2020.
Washington University vascular surgeons treat patients with all forms of vascular disease, including diabetes and peripheral artery disease, in the St. Louis region. It is the section’s mission to provide the highest quality of care to all patients. The CDC notes that patients from historically underserved populations are at increased risk of peripheral arterial disease and other vascular diseases. The section aims to address this disparity through inclusive training and access to quality vascular care in St. Louis communities.
Vascular Surgery Section Chief Luis Sanchez, MD, recognizes the importance of training and hiring vascular surgeons equipped to provide comprehensive care for these patient populations.
“We have to mirror the populations we serve,” says Sanchez, who is the Gregorio A. Sicard Distinguished Professor of Vascular Surgery. “Having physicians who understand the needs and experiences of our patients is critical to providing the highest quality of care. Our training programs reflect that vital mission.”


A Revolution in Patient Care
The Washington University and Barnes-Jewish Heart & Vascular Center offers advanced care for pulmonary embolisms at one of the best hospitals for cardiology, heart surgery and pulmonology, according to U.S. News & World Report. Washington University vascular surgeons are improving care pathways and treatment options for patients with pulmonary embolism and deep vein thrombosis through multidisciplinary collaboration and clinical research.
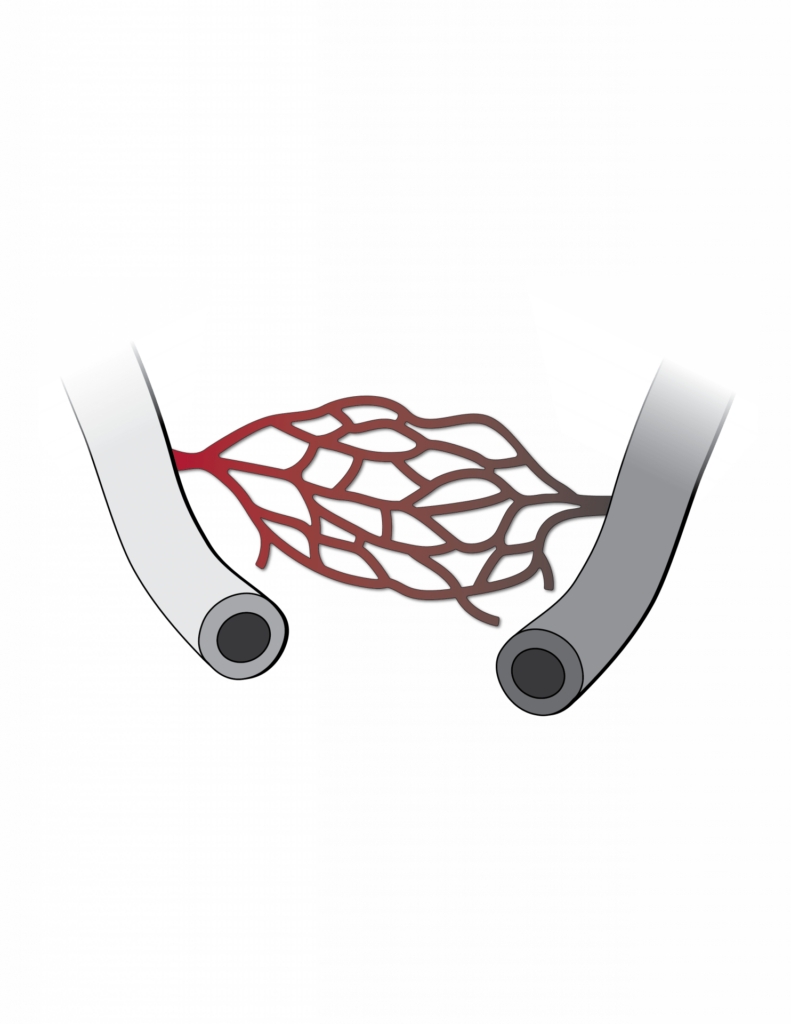
Venous diseases, such as venous insufficiency and deep vein thrombosis (DVT), can be life-and limb-threatening. DVT blood clots that break off and travel to the lungs are the most common cause of pulmonary embolism (PE). The CDC estimates that up to 100,000 people in the United States die from venous thromboembolism (DVT/PE) each year. While blood clots can form slowly, many cases of PE require emergency treatment to reduce the risk of life-threatening complications.
“Pulmonary embolism care at WashU/BJH has undergone a complete revolution over the last few years with the introduction of new technologies that allow for long volume clot extraction percutaneously,” says Washington University vascular surgeon Westley Ohman, MD. “This has been coupled with a multidisciplinary group spanning vascular surgery, interventional radiology, pulmonary, cardiology, ED, critical care, and the eICU to allow us to facilitate timely and appropriate care for patients at BJH and within the broader BJC network. The Pulmonary Embolism Response Team (PERT) allows for a 24/7 access to experts to develop the best care pathway for the individual patients.”
When a patient presents with emergency PE, the PERT, developed by Ohman and a multidisciplinary team of Washington University Physicians, leaps into action.
The best way to avoid fatal DVT/PE is to treat DVT before it leads to PE or another urgent problem. Washington University vascular surgeons, including Ohman and Vipul Khetarpaul, MD, have established practices treating DVT with the most advanced devices available for removing or breaking up blood clots. Clot retrieval devices and other forms of vascular intervention provide minimally invasive options for many patients with DVT/PE.
An upcoming clinical trial will study a new device for percutaneous mechanical thrombectomy in patients with DVT. Led at the School of Medicine by Khetarpaul, the BOLT study could introduce new treatment options for DVT patients.
“Deep venous disease management is rapidly evolving and cutting-edge treatment options are being offered at Washington University,” says Khetarpaul. “The Vascular Surgery Section is involved with several trials including an upcoming trial offering single stage intervention for extensive leg clots using a new device that can rapidly clear the vein clots without need for clot busting medications and multiple interventions.”