
Building on a successful history, this section continues its role as a leader in research and treatment in all aspects of colorectal surgery. Working with gastroenterologists, surgeons provide comprehensive care to patients with diseases of the colon, rectum and anus. Faculty have special expertise in laparoscopic colon surgery, offering this treatment for colon and rectal cancer, diverticulitis, ulcerative colitis, Crohn’s disease, colon polyps, rectal prolapse and chronic constipation. Surgeons apply basic science research to the clinical realm and offer several colorectal cancer clinical trials. This section also offers a one-year colorectal surgery fellowship.
2,787
Operating room cases
19,268
Visits
7
Faculty
1,361
Office procedures
35
Clinical research studies
$416,002
Research funding
Section of Colon and Rectal Surgery | 2021 Annual Report

Patient safety initiatives have long been a priority for the Section of Colon and Rectal Surgery. Recent efforts have reduced surgical site infections, improved recovery after surgery and shortened postoperative length of stay. As the section continues to lead in colorectal cancer care, Washington University colon and rectal surgeons aim to improve outcomes for patients across the region.
Young-onset colorectal cancer is a growing problem. Colorectal cancer is considered young onset if it starts before age 45. Colonoscopy and other prevention and detection methods have led to an overall decrease in colorectal cancer incidence since 1980, yet many patients are being diagnosed with the disease earlier in life. The rate of colorectal cancer in patients 49 and younger has increased by more than 50% in recent years. By 2030, cases of colorectal cancer in people under 50 are expected to nearly double.
Section of Colon and Rectal Surgery Highlights | 2021 Annual Report

Clinical
Washington University colon and rectal surgeon Sean Glasgow, MD, has established a successful peritoneal surface disease program that sees patients from across the Midwest. Peritoneal malignancy is a rare form of cancer that forms in the tissue lining, the abdominal wall and most organs in the abdomen. Glasgow offers the most advanced treatments for peritoneal cancer, including cytoreduction with HIPEC (heated intraperitoneal chemotherapy), which involves removing all visible tumors before applying chemotherapy directly to the peritoneal cavity to kill any remaining cancer. Glasgow has recently partnered with surgical oncologist Beth Helmink, MD, PhD, to continue growing the peritoneal disease program.

Research
Over one million people in the United States have inflammatory bowel disease (IBD). For patients with these often-debilitating conditions, including ulcerative colitis, the goal of treatment is to return to a normal quality of life. The Section of Colon and Rectal Surgery is part of a multicenter American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) Collaborative focused on IBD. As part of the collaborative, Washington University colorectal surgeons are refining quality measurements for ulcerative colitis surgery and investigating the impact of immunosuppressive therapy on patient outcomes, to improve quality of life for all patients with IBD.
Education
For over 40 years, the Washington University Colorectal Surgery Fellowship has offered advanced training in a high volume of complex cases. Led by Program Director Matthew Silviera, MD, MS, and Associate Program Director Radhika Smith, MD, the one-year fellowship provides experience in open, laparoscopic and robotic surgery. Fellows develop autonomy while working closely with seven board-certified colorectal surgeons, as well as gastroenterologists, pathologists, medical and radiation oncologists, enterostomal therapists, and other professionals. The program trains three fellows each year and includes in-depth exposure to all aspects of colorectal disease and surgery, including the latest treatments for colon and rectal cancer.

Regional Leaders in Colorectal Cancer Care
Patient safety initiatives have long been a priority for the Section of Colon and Rectal Surgery. Recent efforts have reduced surgical site infections, improved recovery after surgery and shortened postoperative length of stay. As the section continues to lead in colorectal cancer care, Washington University colon and rectal surgeons aim to improve outcomes for patients across the region.
Preoperative interventions have the potential to improve outcomes for patients at risk for postoperative complications. A recent retrospective study led by general surgery residents Ebun Otegbeye, MD, and William Chapman Jr., MD, MPHS, examined PROMIS (Patient-Reported Outcomes Measurement Information System) physical function scores, finding that patients who reported severe disability were at an increased risk of complications. The ability to identify these patients before surgery, using PROMIS scores, enables surgeons to provide targeted preoperative interventions to improve surgical outcomes.
The section, which has developed and refined patient education materials in recent years, is an early adopter of the Department of Surgery Surgical Prehabilitation and Readiness (SPAR) Program. SPAR helps patients improve their health before surgery by providing them with tools and resources— such as nutritional information, an incentive spirometer and exercise goals.
Other recent studies from the section have examined the impact of delayed treatment, travel time and fragmentation of care.
“Many of our patients come from over 100 miles away,” says Colon and Rectal Surgery Section Chief Matthew Mutch, MD, the Solon and Bettie Gershman Professor of Surgery. “We have a truly regional presence and are taking active steps to provide the best care for all patients, no matter where they come from.”
To best serve colorectal cancer patients region-wide, the section is building relationships in local communities and increasing its presenceat locations across the St. Louis area. Mutch serves as chief of surgery at Barnes- Jewish West County Hospital, where Matthew Silviera, MD, MS, and Radhika Smith, MD, continue to grow their practices. Colorectal surgeons, including Sean Glasgow, MD, and Steven Hunt, MD, see patients at the Center for Advanced Medicine –South County. Kerri Ohman, MD, expands colorectal cancer care to patients in North St. Louis County at Christian Hospital. At the Center for Advanced Medicine, General Surgery Residency Program Director Paul Wise, MD, specializes in inherited colorectal cancer and hereditary colorectal cancer syndromes.
“In the coming years, we will continue to improve access to optimal, unified colorectal cancer care to patients across the region,” says Mutch.
Fighting Young-onset Colorectal Cancer
Young-onset colorectal cancer is a growing problem. Colorectal cancer is considered young onset if it starts before age 45. Colonoscopy and other prevention and detection methods have led to an overall decrease in colorectal cancer incidence since 1980, yet many patients are being diagnosed with the disease earlier in life. The rate of colorectal cancer in patients 49 and younger has increased by more than 50% in recent years. By 2030, cases of colorectal cancer in people under 50 are expected to nearly double.
“Patients with young-onset colorectal cancer face a unique set of social, biological and financial challenges,” says Chief of Colon and Rectal Surgery Matthew Mutch, MD. “From finding childcare and scheduling visits while working full time, to paying for treatment and understanding genetic factors, this patient population has specific biopsychosocial needs.”
Washington University colorectal surgeons, medical and radiation oncologists, and other specialists are partnering with Barnes-Jewish Hospital and Siteman Cancer Center to meet the needs of young-onset colorectal cancer patients through multidisciplinary care.
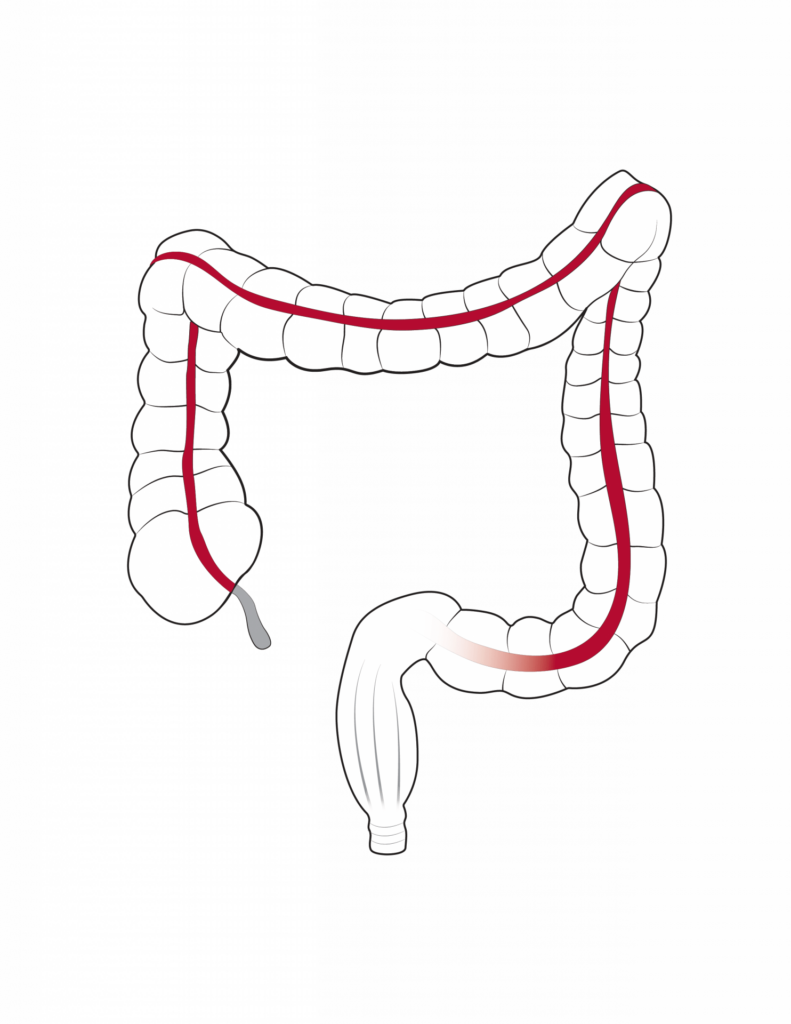
The Section of Colon and Rectal Surgery has implemented a new standard of care for rectal cancer patients, using neoadjuvant short course radiation therapy, followed by either nonoperative management or surgery. This expertise, combined with similar advances in treatment and understanding of colon cancer, has established Washington University and Siteman Cancer Center as leaders in the treatment of colorectal cancer.
Mutch is collaborating with medical oncologist Katrina Pedersen, MD, and radiation oncologist Hyun Kim, MD, to formalize a program for young-onset colorectal cancer patients. The program will include top cancer care, access to social and genetic counseling resources, and patient education through community outreach, as well as research to determine causes of young-onset colorectal cancer and potential markers for future therapies. Research partnerships between the section and faculty from the Division of Public Health Sciences aim to address the biopsychosocial issues particular to young-onset colorectal cancer.
“We have seen incredible progress in the fight against colorectal cancer overall,” says Mutch. “It’s time we do the same for younger patients as well.”